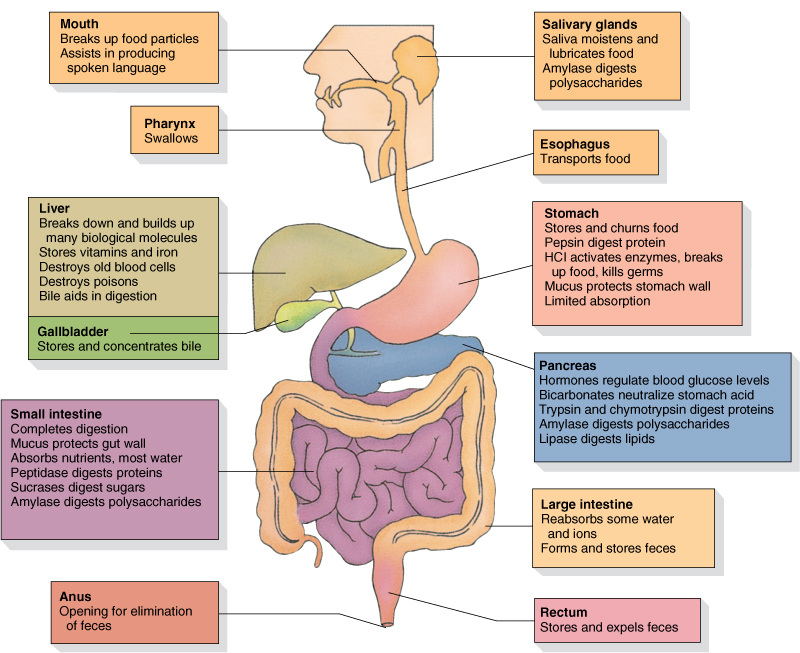
Functions of the Digestive System:- Ingestion of food
- Digestion of food
- Absorption of nutrients
- Elimination of wastes
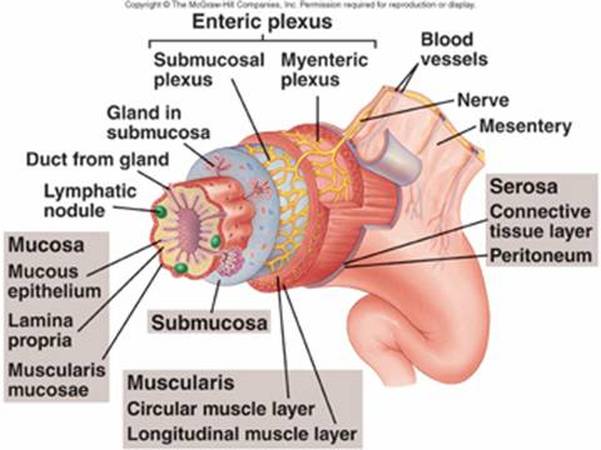
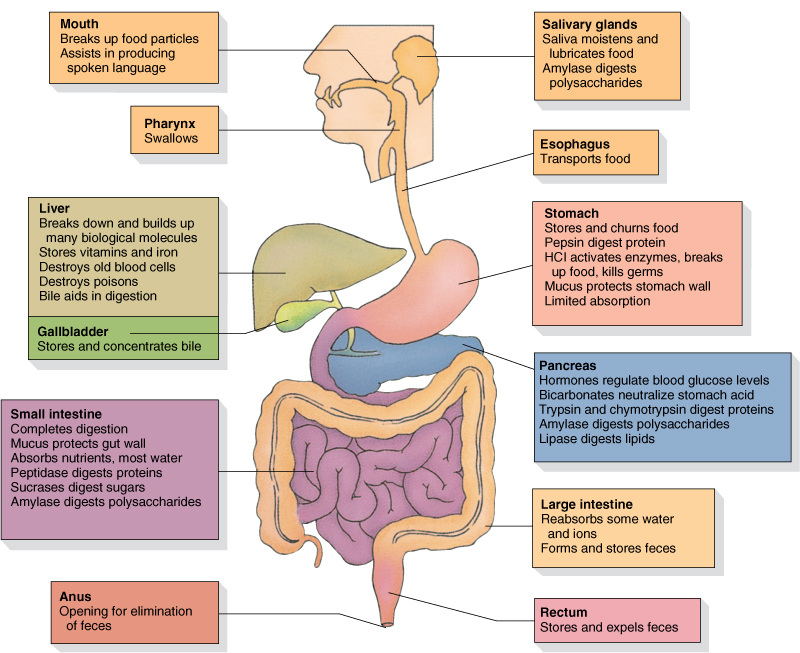 Organs of the Digestive Tract and their Functions 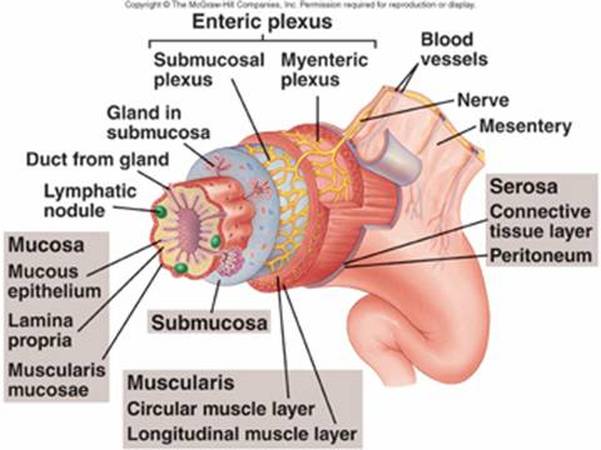 Digestive Tract Histology Histology of the Digestive System: - The innermost tunic, the mucosa, consists of mucous epithelium, a loose connective tissue called the lamina propria, and a thin smooth muscle layer, the muscularis mucosae.
- The submucosa lies just outside the mucosa. It is a thick layer of loose connective tissue containing nerves, blood vessels, and small glands. An extensive network of nerve cell processes forms a plexus (network). Autonomic nerves innervate this plexus.
- The next tunic is the muscularis. In most parts of the digestive tract it consists of an inner layer of circular smooth muscle and an outer layer of longitudinal smooth muscle. Another nerve plexus, also innervated by autonomic nerves, lies between the two muscle layers. Together, the nerve plexuses of the submucosa and muscular is compose the enteric nervous system.
- The fourth, or outermost, layer of the digestive tract is either a serosa or an adventitia. The serosa consists of the peritoneum, which is a smooth epithelial layer, and its underlying connective tissue. Regions of the digestive tract not covered by peritoneum are covered by a connective tissue layer called the adventitia, which is continuous with the surrounding connective tissue.
Teeth:
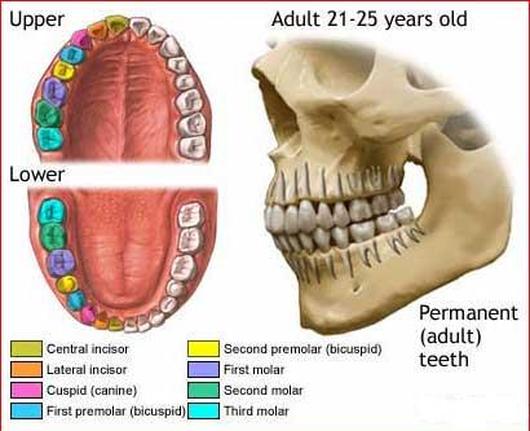
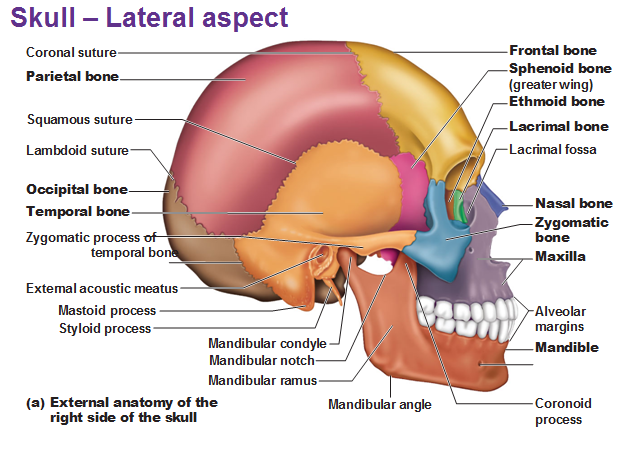
There are 32 teeth in the normal adult mouth, located in the mandible and maxillae. The teeth can be divided into quadrants: right upper, left upper, right lower, and left lower. In adults, each quadrant contains one central and one lateral incisor; first and second premolars; and first, second, and third molars. The thirst molars are called wisdom teeth.
The teeth of adults are called permanent teeth, or secondary teeth. Most of them are replacements for the 20 primary teeth, or deciduous teeth, also called milk or baby teeth, which are lost during childhood.
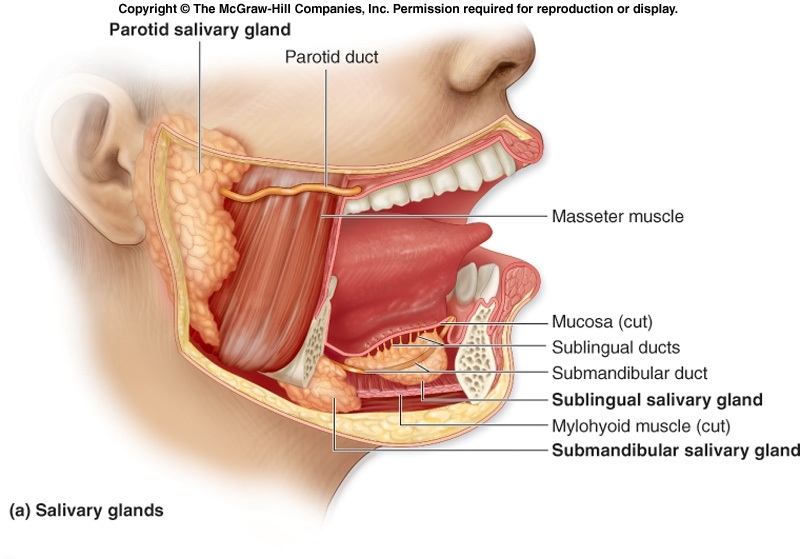
Each tooth consists of a crown with one or more cusps (points), a neck, and a root. The center of the tooth is a pump cavity, which is filled with blood vessels, nerves, and a connective tissue, called pulp. The pulp cavity is surrounded by a living, cellular, bonelike tissue called dentin. The dentin of the tooth crown is covered by an extremely hard, acellular substance called enamel, which protects the tooth against abrasion and acids produced by bacteria in the mouth. The surface of the dentin in the root is covered with cementum, which helps anchor the tooth in the jaw. Salivary Glands:- Parotid Gland- serous glands located just anterior to each ear. Parotid ducts enter the oral cavity adjacent to the second upper molars.
- Submandibular Glad- produce more serous than mucous secretions. Each gland can be felt as a soft lump along the inferior border of the mandible. The submandibular ducts open into the oral cavity on each side of the frenulum of the tongue.
- The sublingual glands- the smallest of the three paired salivary glands, produce primarily mucous secretions. They lie immediately below the mucous membrane in the floor of the oral cavity. Each sublingual gland has 10-12 small ducts opening onto the floor of the oral cavity.
Events During the Three Phases of Swallowing: - During the voluntary phase, a bolus of food is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx.
- During the pharyngeal phase, the soft palate is elevated, closing off the nasopharynx. The pharynx and larynx are elevated.
- Successive constriction of the pharyngeal constrictors from superior to inferior forces the bolus through the pharynx and into the esophagus. As this occurs, the vestibular and vocal folds expand medially to close the passage of the larynx. The epiglottis is bent down over the opening of the larynx largely by the force of the bolus pressing against it.
- As the inferior constrictor contracts, the upper esophageal sphincter relaxes, allowing the bolus to enter the esophagus.
- During the esophageal phase, the bolus is moved by peristaltic contractions of the esophagus toward the stomach
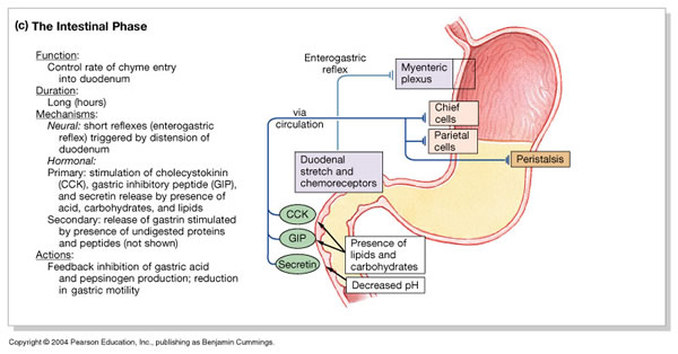
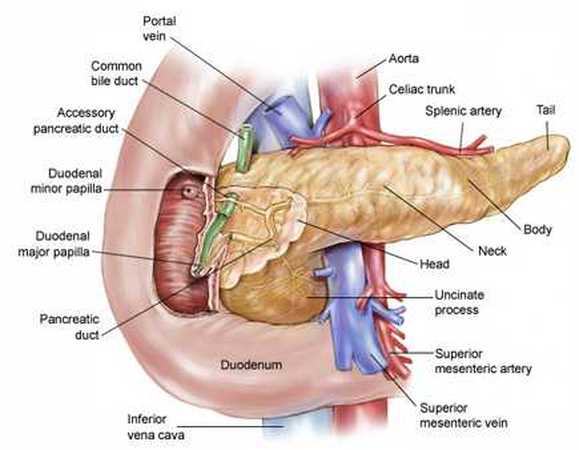
Flow of Bile and Pancreatic Secretions through the Duct system of the Liver, Gallbladder, & Pancreas:- The hepatic ducts from the liver lobes combine to form the common hepatic duct.
- The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct.
- The common bile duct joins the pancreatic duct.
- The combined duct empties into the duodenum at the duodenal papilla.
- Pancreatic secretions may also enter the duodenum through an accessory pancreatic duct, which also empties into the duodenum.
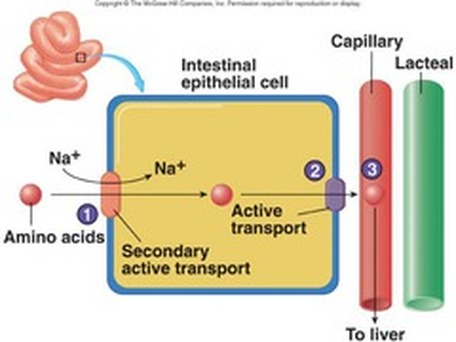
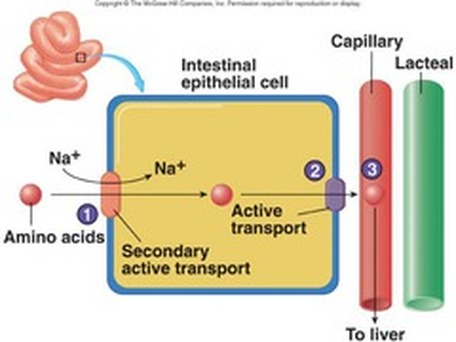 Lipid Transport across intestinal epithelium Lipid Transport:- Bile salts surround fatty acids and monoglycerides to form micelles.
- Micelles attach to the cell membranes of intestinal epithelial cells, and the fatty acids and monoglycerides pass by simple diffusion into the intestinal epithelial cells.
- Within the intestinal epithelial cell, the fatty acids and monoglycerides are converted to triglycerides; proteins coat the triglycerides to form chylomicrons, which move out of the intestinal epithelial cells by exocytosis.
- The chylomicrons enter lacteals of the intestinal villi and are carried through the lymphatic system to the general circulation.
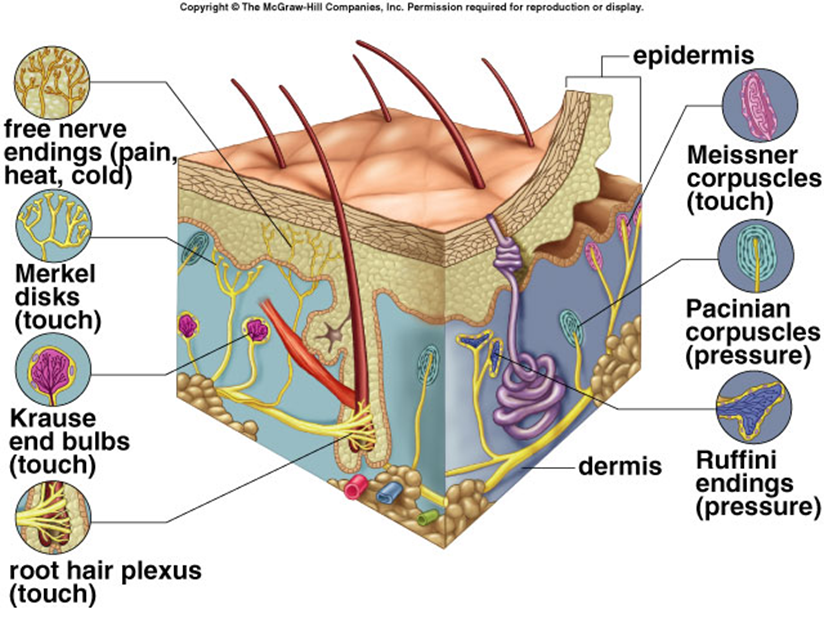
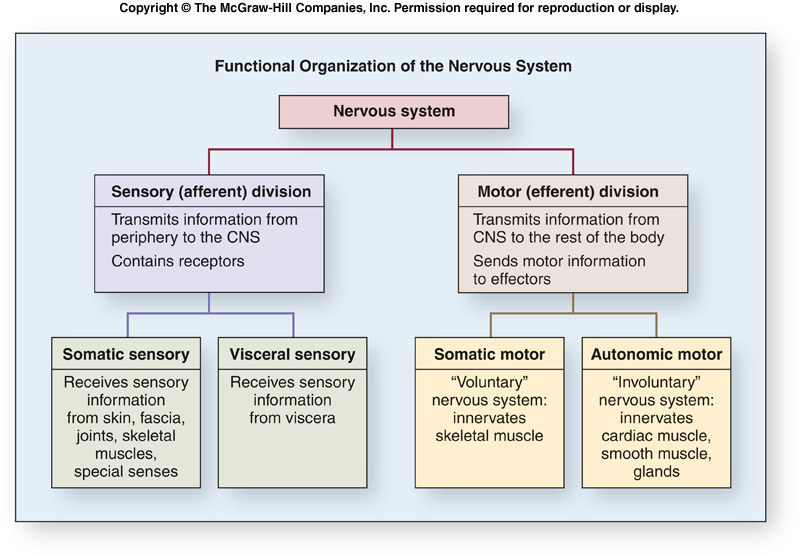
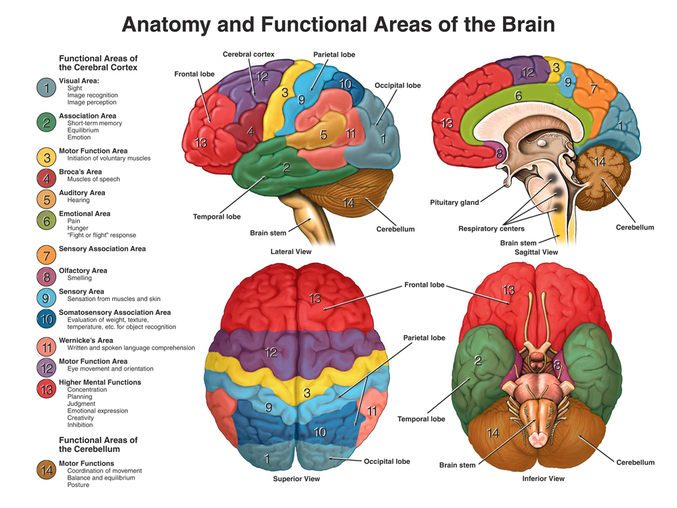
Sense is the ability to perceive stimuli. The senses are the means by which the brain receives information about the environment and the body. Sensation, or perception, is the conscious awareness of stimuli received by sensory receptors.
Historically five senses are recognized: smell, taste, sight, hearing, and touch. Today we recognize many more senses and divide them into two basic groups:general and special senses. The general senses have receptors distributed over a large part of the body. They are divided into two groups: the somatic senses and the visceral senses. The somatic senses provide sensory information about the body and the environment. The visceral senses provide information about various internal organs, primarily involving pain and pressure.
Special senses are more specialized in the structure and are localized to specific parts of the body. THe special senses are sell, taste, sight, hearing, and balance. General Senses
The General senses are widely distributed though out the body an include the senses of touch, pressure, pain, temperature, vibration, itch, and proprioception,, which is the sense of movement and position of the body and limbs.
Sensory receptors are sensory nerve endings or specialized cells capable of responding to stimuli by developing action potentials. Several types of receptors are associated with both the social and the general senses, and each responds to a different type of stimulus:
Mechanoreceptors respond to mechanical stimuli, such as the bending or stretching of receptors.
Chemoreceptors respond to chemicals, such as odor molecules.
Photoreceptors respond to light.
Thermoreceptors respond to temperature changes.
Nociceptors respond to stimuli that result in the sensation of pain.
Free Nerve Endings are the most common receptors and are relatively unspecialized neuronal branches that are similar to dendrites. Free nerve endings are distributed throughout almost all parts of the body. Some free nerve endings respond to painful stimuli, some to temperature, some to itch, and some to movement.
Cold Receptors or Warm Receptors are receptors for temperature. Cold receptors respond to decreasing temperatures but stop responding at temperatures below 12 C. Warm receptors respond to increasing temperatures but stop responding at temperatures about 47 C. It is sometimes difficult to distinguish very cold from very warm objects touching the skin because only pain receptors are stimulated at temperatures below 12 C or above 47 C.
Touch Receptors are structurally more complex than free nerve endings, and many are enclosed by capsules. There are several types of touch receptors: Merkel disks are small, superficial nerve endings involved in detecting light touch and superficial pressure. Hair follicle receptors, associated with hairs, are also involved in detecting light touch. LIght touch receptors are very sensitive but not very discriminative, meaning that the point being touched cannot be precisely located. Receptors for fine, discriminative touch, called Meissner corpuscles, are located just deep to the epidermis. These receptors are very specific in localizing tactile sensations. Deeper tactile receptors, called Ruffini corpuscles play an important role in detecting continuous pressure in the skin. The deepest receptors are associated with tendons and joints and are called pacinian corpuscles. These receptors relay information concerning deep pressure, vibration, and position (proprioception).
Special Senses
The senses of smell, taste, sight, hearing, and balance are associated with very specialized, localized sensory receptors. The sensations of smell and taste are closely related, both structurally and functionally, and both are initiated by the interaction of chemicals with sensory receptors. The sense of vision is initiated by the interaction of light with sensory receptors. Both hearing and balance function in response to the interaction of mechanical stimuli with sensory receptors. Hearing occurs in response to sound waves, and balance occurs in response to gravity or motion.
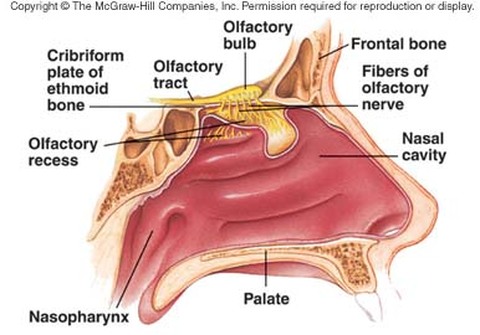
Olfaction is the sense of smell, and occurs in response to airborne molecules, called odorants, that enter the nasal cavity. Olfactory neurons are bipolar neurons within the olfactory epithelium, which lines the superior part of the nasal cavity.
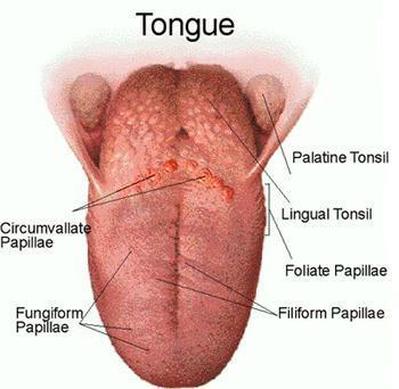
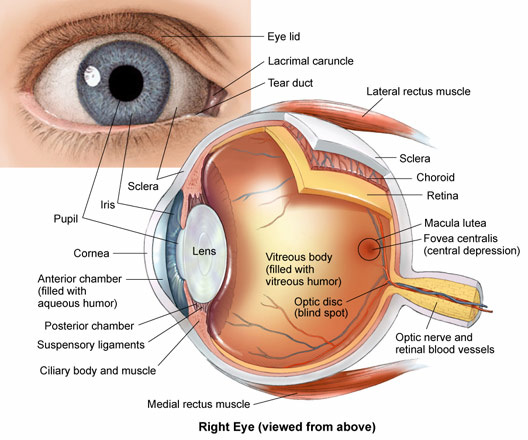
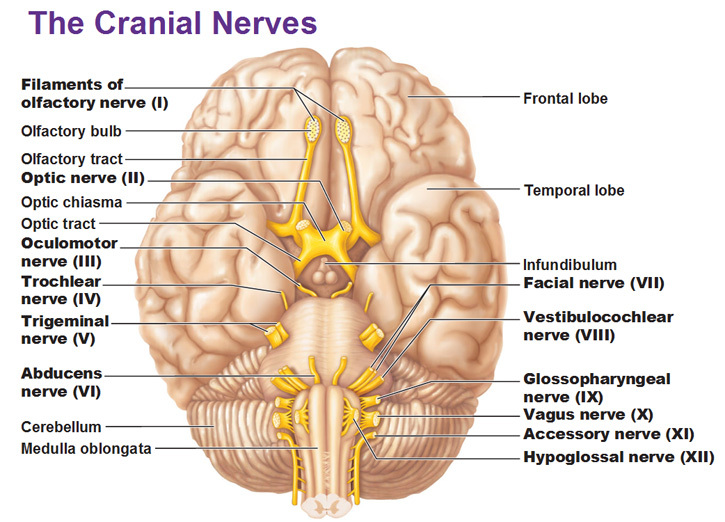
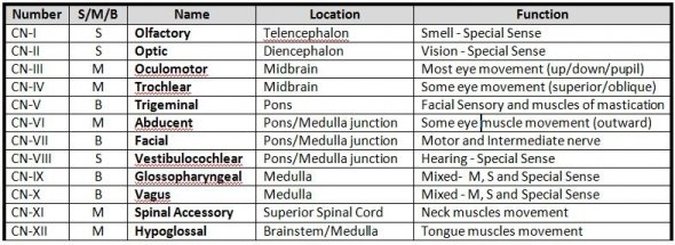
Axons from olfactory neurons form the olfactory nerves (cranial nerve I), which pass through foramina of the cribiform plate and enter the olfactory bulb. There they synapse with interneurons that relay action potentials to the brain through the olfactory tracts. Each olfactory tract terminates in an area of the brain called the olfactory cortex, located within the temporal and frontal lobes. Olfaction is a major sensation that is relayed directly to the cerebral cortex without first passing through the thalamus. The sensory structures that detect taste stimuli are the taste buds. Taste buds are oval structures located on the surface of certain papillae, which are enlargements on the surface of tongue. Taste buds are also distributed throughout other areas of the mouth and pharynx, such as on the palate, the root of the tongue, and the epiglottis. Each taste bud consists of two types of cells. Specialized epithelial cells form the exterior supporting capsule of each taste bud, and the interior consists of about 40 taste cells. Each taste cell contains hairlike processes, called taste hairs, that extend into a tiny opening in the surrounding stratified epithelium, called a taste pore. Eyelids with their associated lashes, protect the eyes from foreign objects. If an object suddenly approaches the eye, the eyelids protect the eye by closing and then opening quite rapidly (blink reflex). Blinking, which normally occurs about 20 times per minute, also helps keep the eyes lubricated by spreading tears over the surface.
The conjunctiva is a thin, transparent mucous membrane covering the inner surface of the eyelids and the anterior surface of the eye. The secretions of the conjunctiva help lubricate the surface of the eye. Conjunctivitis is an inflammation of the conjunctiva.
The lacrimal apparatus consists of a lacrimal gland situated in the superior lateral corner of the orbit and a nasolacrimal duct and associated structures in the inferior medial corner of the orbit. The lacrimal gland produces tears, which pass over the anterior surface of the eye. Most of the fluid produced by the lacrimal glands evaporates from the surface of the eye, but excess tears are collected in the medial angle of the eyes by small ducts called lacrimal canaliculi. These canaliculi open into a lacrimal sac, an enlargement of the nasolacrimal duct, which opens into the nasal cavity. Tears lubricate and cleanse the eye. They also contain an enzyme that helps combat eye infections.
Movement of each eyeball is accomplished by six skeletal muscles called the extrinsic eye muscle. For of these muscles run more or less straight from their origins in the posterior portion of the orbit to their insertion sites on the eye, to attach to the four quadrants of the eyeball. They are the superior, inferior, medial, and lateral rectus muscles. Two muscles, the superior and inferior oblique muscles, are located to an angle to the long axis of the eyeball. The outer segments of rod and cone cells are modified by numerous foldings of the cell membrane to form discs. Rod cells contain photosensitive pigment called rhodopsin, which is made up of the colorless protein opsin in loose chemical combination with a yellow pigment called retinal.
Visual Pathways
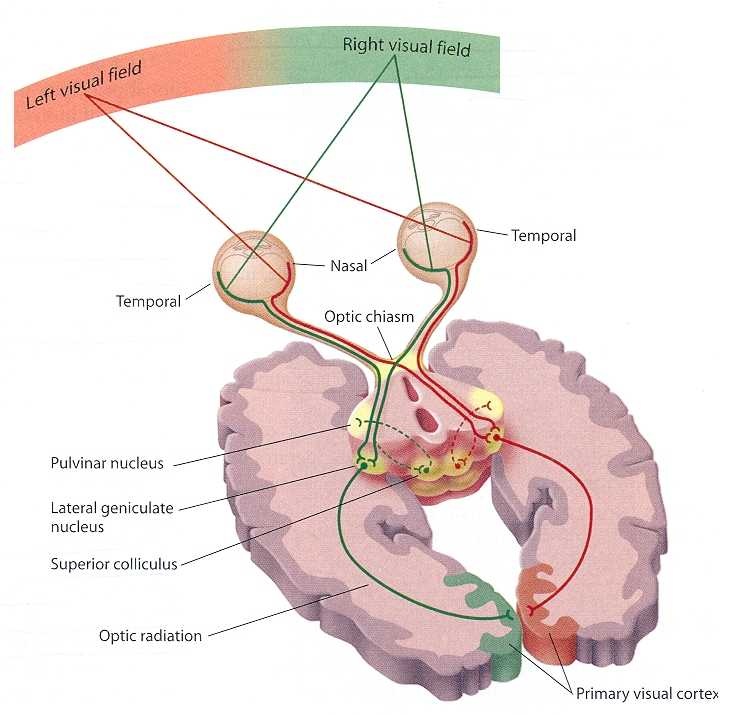
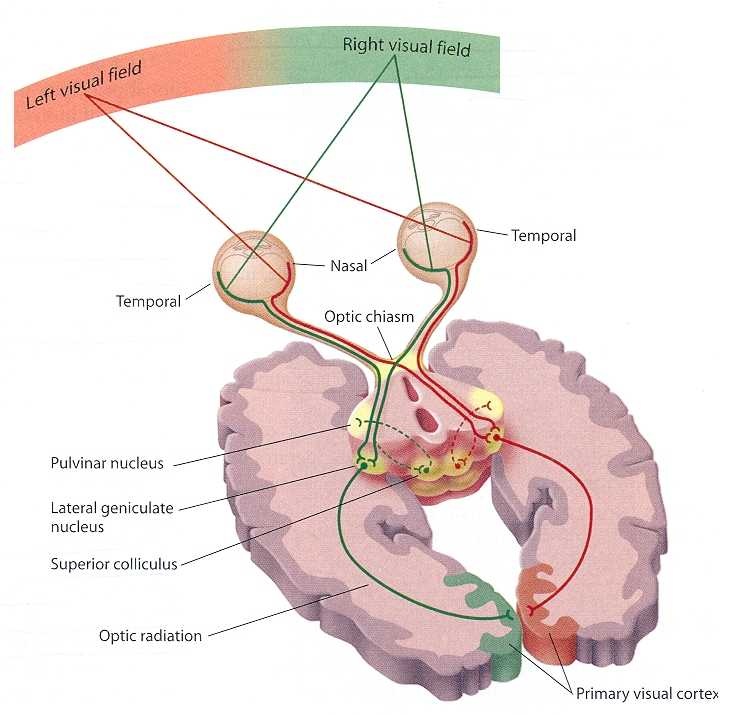
Neuronal Pathways for Vision - Each visual field is divided into temporal and nasal halves.
- After passing through the lens, light from each half of a visual fields projects to the opposite side of the retina.
- An optic nerve consists of axons extending from the retina to the optic chasm.
- In the optic chasm, axons from the nasal part of the retina cross and project to the opposite side of the brain. Axons from the temporal part of the retina do not exist.
- An optic tract consists of axons that have passed through the optic chasm (with or without crossing) to the thalamus.
- The axons synapse in the thalamus. Collateral branches of the axons in the optic tracts synapse in the superior colliculi.
- An optic radiation consists of axons from thalamic neurons that project to the visual cortex.
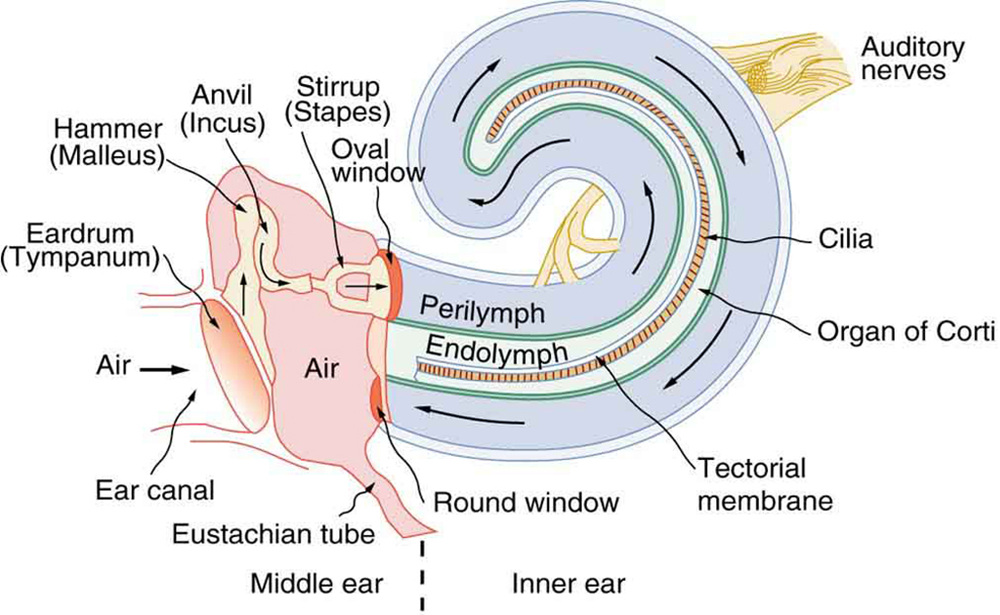
Effect of Sound Waves o Middle and Inner Ear Structures
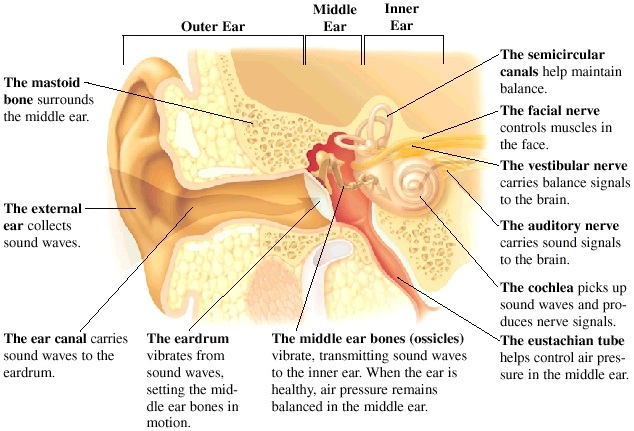
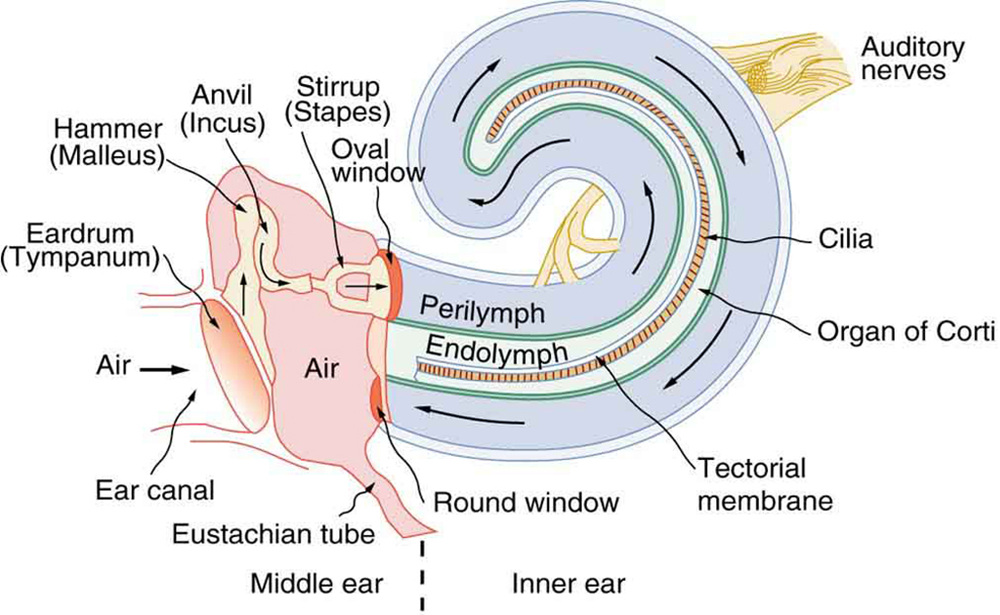
Hearing- Sound waves strike the tympanic membrane and cause it to vibrate
- Vibration of the tympanic membrane causes the malleus, the incus, and the stapes to vibrate
- The foot plate of the stapes vibrates in the oval window
- Vibration of the foot palate causes the perilymph in the scala vestibule to vibrate
- Vibration of the perilymph causes the vestibular membrane to vibrate, which causes vibrations in the endolymph.
- Vibration of the endolymph causes displacement of the basilar membrane. Short waves (high pitch), causes displacement of the basilar membrane near the coal window, and longer waves (low pitch) cause displacement of the basilar membrane some distance from the oval window. Movement of the basilar membrane is detected in the hair cells of the spiral organ, which are attached to the basilar membrane. Vibrations of the perilymph in the scala vestibuli and of the basilar membrane are transferred to the perilymph of the scala tympani.
- Vibrations in the perilymph of the scala tympani are transferred to the round window, where they are dampended.
Functions of the Nervous System- Receiving sensory input. Sensory receptors monitor numerous external and internal stimuli.
- Integrating information. The brain and spinal cord are the major organs for processing sensory input and initiating responses. The input may produce an immediate response, be stored as memory, or be ignored.
- Controlling muscles and glands. Skeletal muscles normally contract only when stimulated by the nervous system. Thus, by controlling skeletal muscle, the nervous system controls the major body movements of the body. The nervous system also participates in controlling cardiac muscle, smooth muscle, and many glands.
- Maintaining homeostasis. This function depends on the nervous system's ability to detect, interpret, and respond to changes in internal and external conditions. In response, the nervous system can stimulate or inhibit the activities of other systems to help maintain a constant internal environment.
- Establishing and maintaining mental activity. The brain is the center of mental activity, including consciousness, memory, and thinking.
Cells of the Nervous System
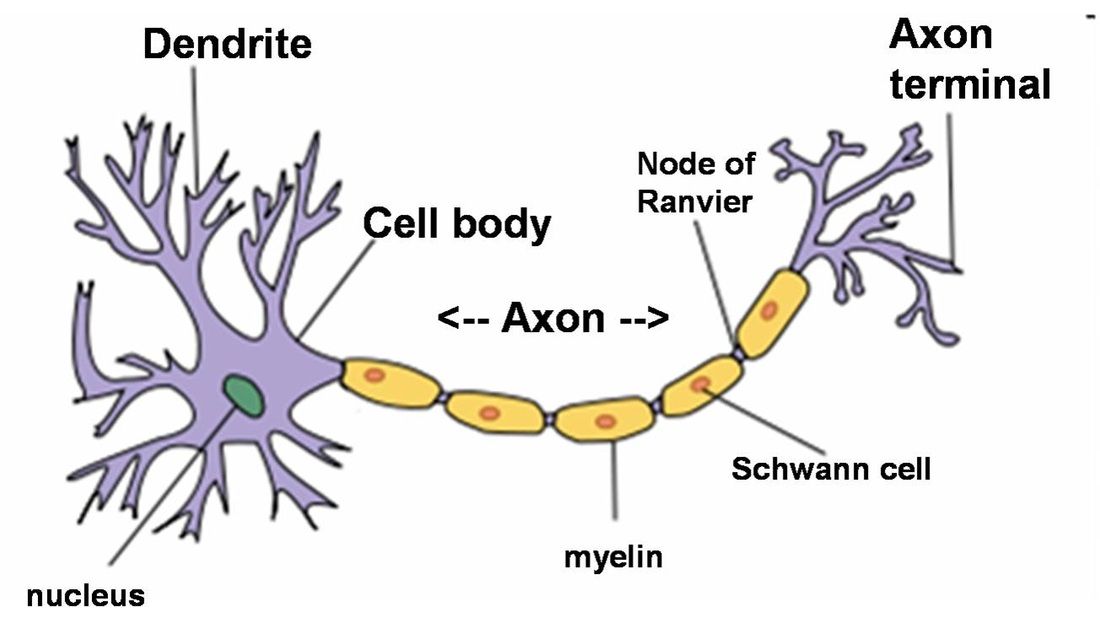
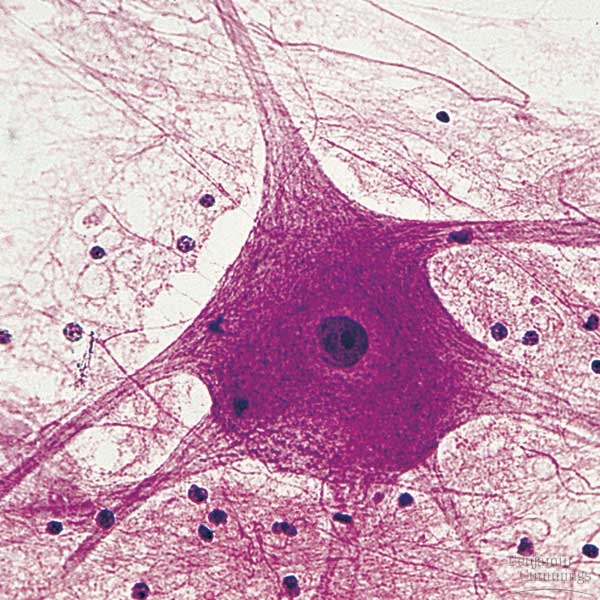
Neurons- or nerve cells, receive stimuli, conduct action potentials and transmit signals to other neurons or effector organs. There are three parts to a neuron: a cell body and two types of processes, called dendrites and axons.
Each neuron cell body contains a single nucleus. As with many other cell, the nucleus of the neuron is the source of information for gene expression.
Dendrites- are short, often highly branching cytoplasmic extensions that are tapered from their bases at the neuron cell body to their tips. Most dendrites are extensions of the neuron cell body, but dendritelike structures also project from the peripheral ends of some sensory axons. Dendrites usually receive information from other neurons or from sensory receptors and transmit the information toward the neuron cell body.
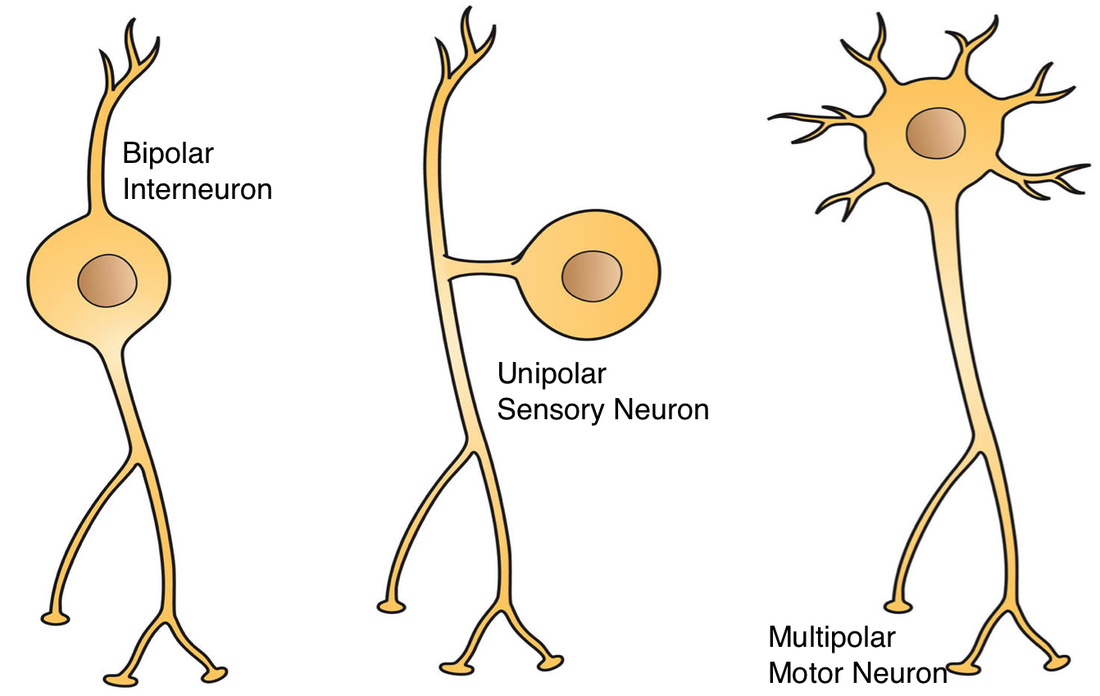
Each neuron has an axon, a single long cell process extending from the neuron cell body. The area where the axon leaves the neuron cell body is called the axon hillock. Each axon has a uniform diameter and may vary in length from a few millimeters to more than a meter. Axons of sensory neurons conduct action potentials towards towards the CNS, and axons of motor neurons conduct action potentials from one part of the brain or spinal cord to another part. An axon may remain unbranched or may branch to form collateral axons. Axons can be surrounded by highly specialized insulating later of cells called the myelin sheath. Types of Neurons:
Multipolar neurons- have many dendrites and a single axon.
Bipolar neurons- have two processes: one dendrite and one axon. Bipolar neurons are located in some sensory organs, such as in the retina of the eye and in the nasal cavity.
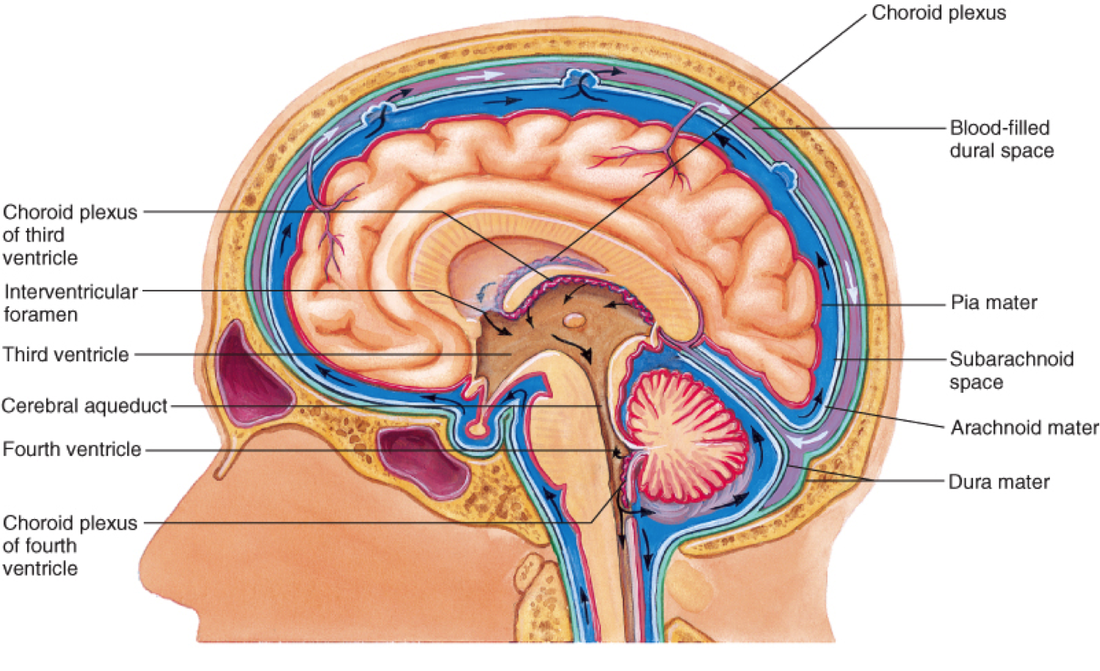
Pseudo-unipolar neurons- have a single process extending from the cell body. This process divides into two processes a short distance from the cell body. One process extends to the periphery, and the other extends to the CNS. The two extensions function as a single axon with small, dendrite like sensory receptors at the periphery. The axon receives sensory information at the periphery and transmits that information in the form of action potentials to the CNS. The Resting Membrane Potential is generated by three main factors: 1.) a higher concentration of K+ immediately inside the cell membrane, 2.) a higher concentration of Na+ immediately outside the cell membrane, and 3.) greater permeability of the cell membrane to K+ than to Na+. Thus, the resting membrane potential results from differences in the concentration of ions across the membrane and the permeability characteristics of the membrane. A Synapse is a junction where the axon of one neuron interacts with another neuron or with cells of an effector organ, such as a muscle or gland. The end of the axons forms a presynaptic terminal. The membrane of the dendrite or effector cell is the postsynaptic membrane, and the space separating the presynaptic and postsynaptic membranes is the synaptic cleft. Chemical substances called neurotransmitters are stored in synaptic vesicles in the presynaptic terminal. Flow of Cerebrospinal Fluid- Cerebrospinal Fluid (CSF) is produced by the choroid plexuses of each of the four ventricles (inset, lower left).
- CSF from the lateral ventricles flows to the third ventricle.
- CSF flows from the third ventricle through the cerebral aqueduct to the fourth ventricle.
- CSF exits the fourth ventricle through openings in the wall of the fourth ventricle and enters the subarachnoid space. Some CSF enters the central canal of the spinal fluid.
- CSF flows through the subarachnoid space to the arachnoid granulations in the superior sagittal sinus, where it enters the venous circulation (inset, upper right).
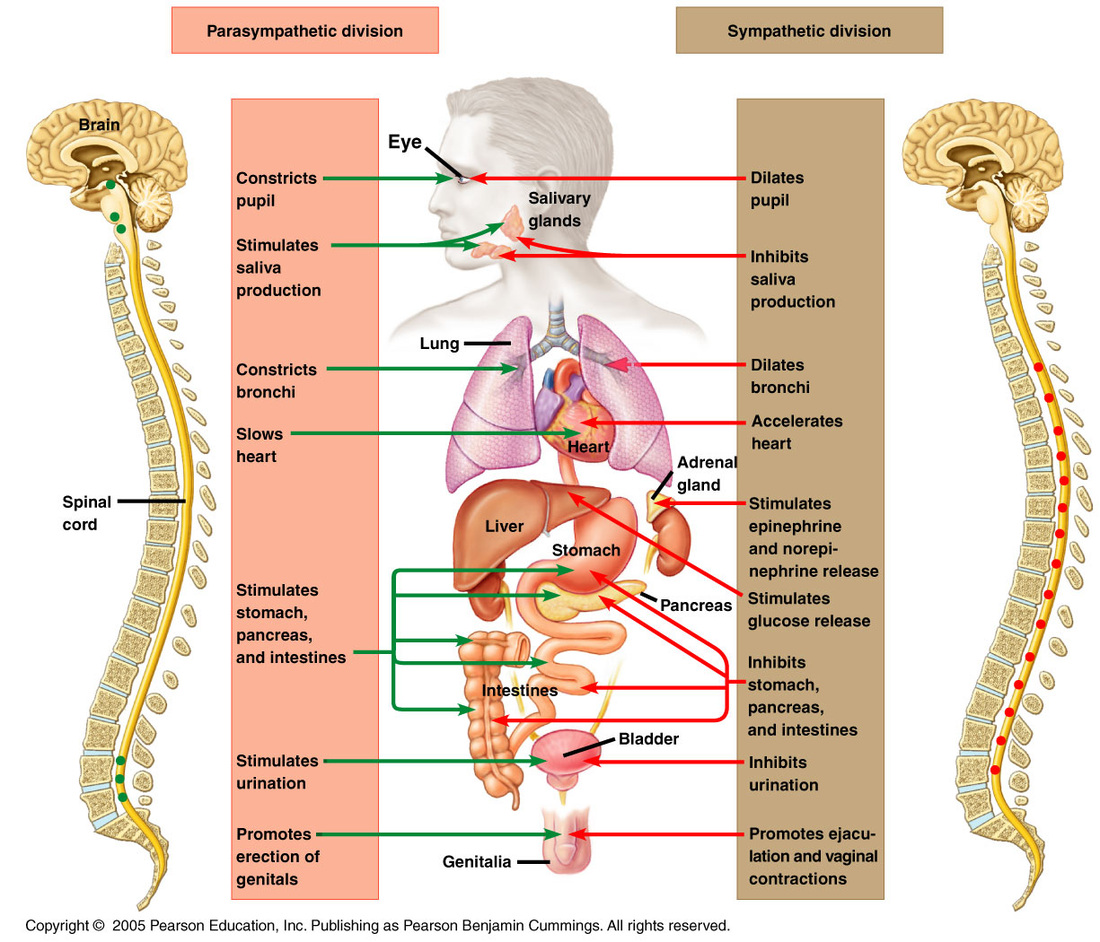
The autonomic nervous system is composed of the sympathetic and the parasympathetic division. Increased activity in sympathetic neurons generally prepares the individual for physical activity, whereas parasympathetic stimulation generally activates involuntary functions, such as digestion, that are normally associated with the body at rest.
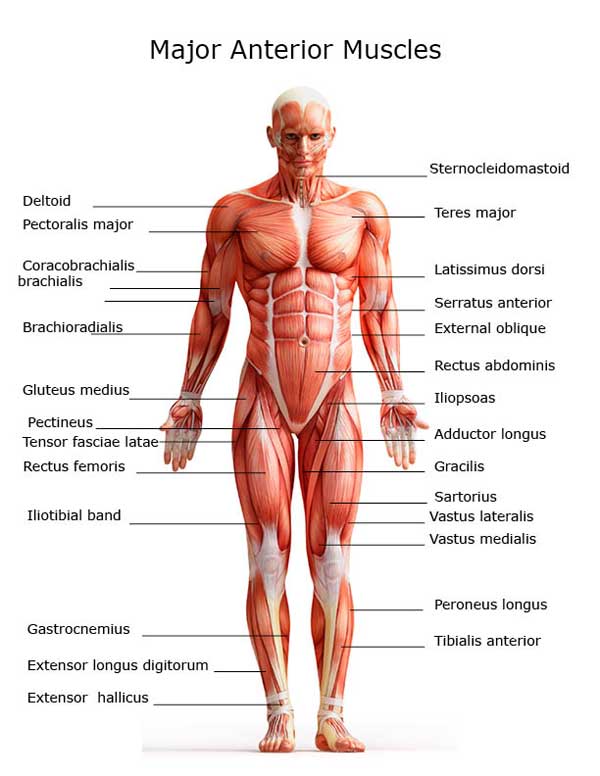
Functions of the Muscular System- Movement of the body
- Maintenance of posture
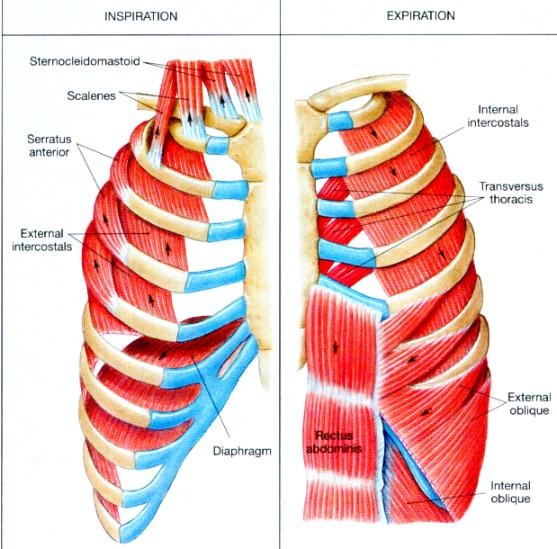
- Respiration
- Production of body heat
- Communication
- Constriction of organs and vessels
- Contraction of the heart
Characteristics of Skeletal Muscle- Contractibility. When skeletal muscles contract, they cause the structures to which they are attacked to move. Skeletal muscles shorten forcefully during contraction, but they lengthen passively. EIther gravity or the contraction of an opposing muscle produces a force that pulls on the shortened muscle, causing it to lengthen.
- Excitability. The capacity of skeletal muscle to respond to a stimulus. Normally, the stimulus is from nerves that we consciously control.
- Extensibility. The skeletal muscles stretch. After a contraction, skeletal muscles can be stretched to their normal resting length and beyond to a limited degree.
- Elasticity. Skeletal muscles are able to recoil to their original resting length after they have been stretched.
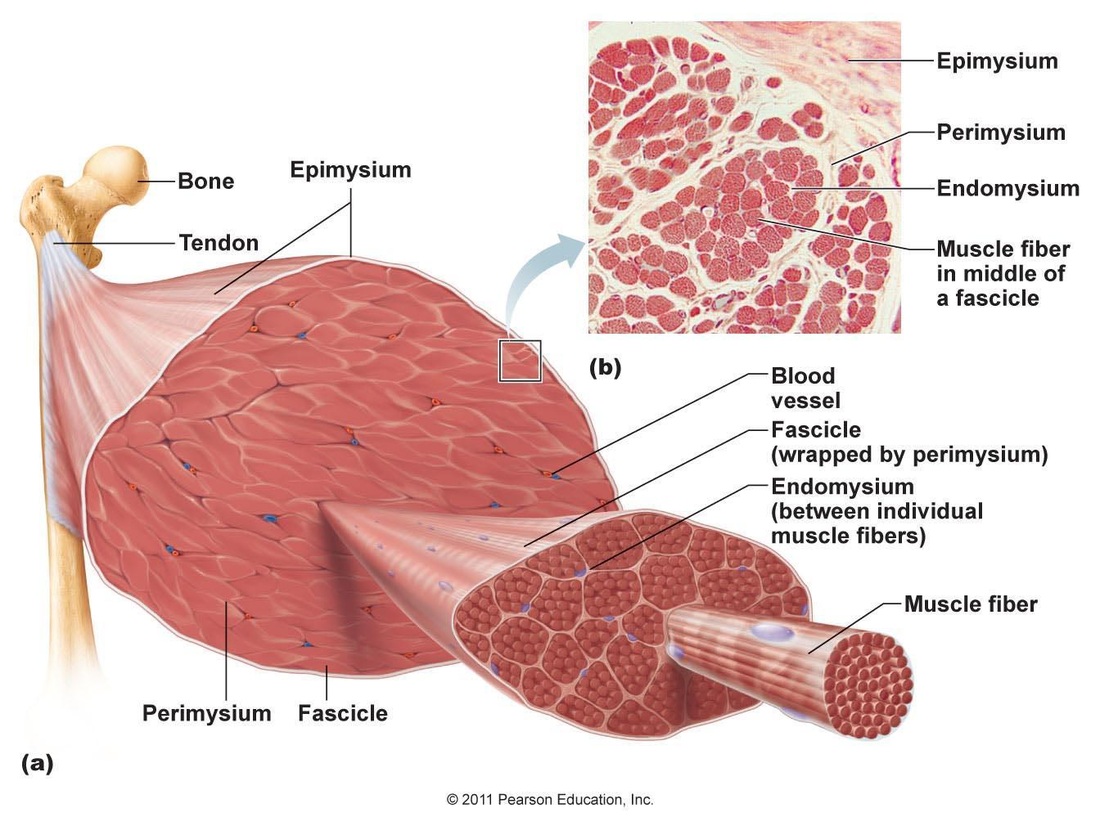
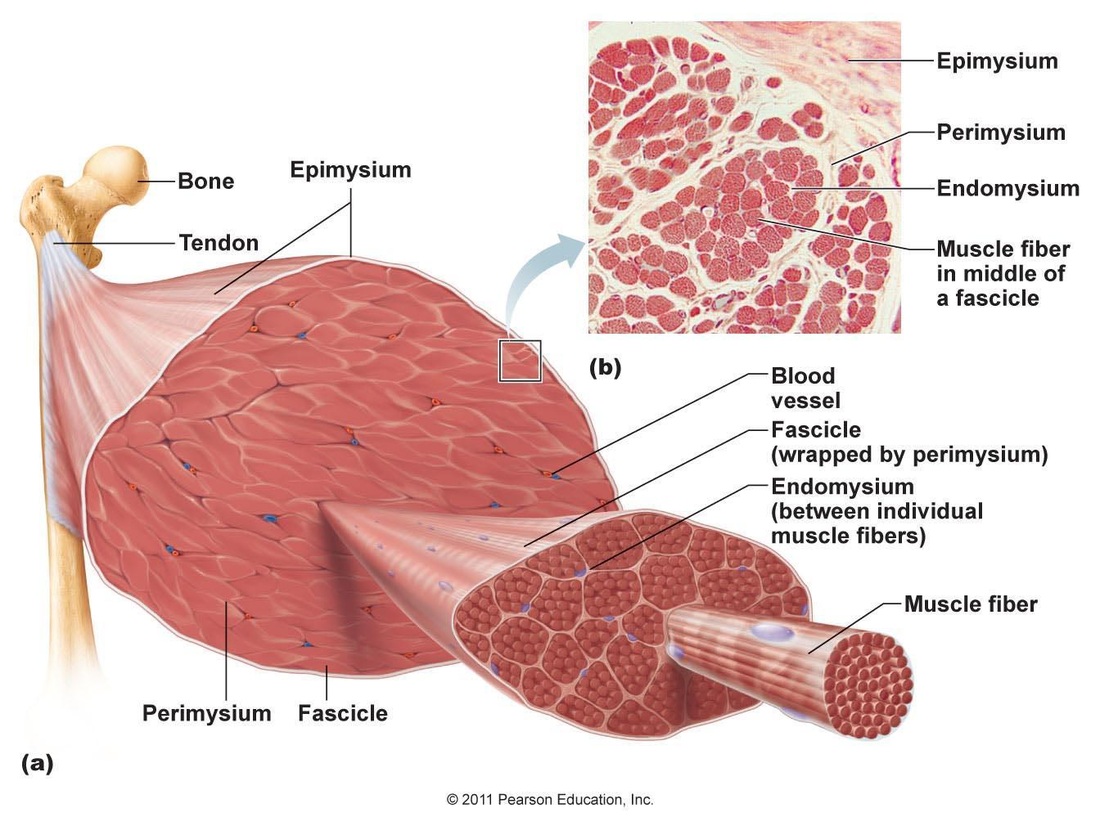
Connective TIssue Coverings of Muscle
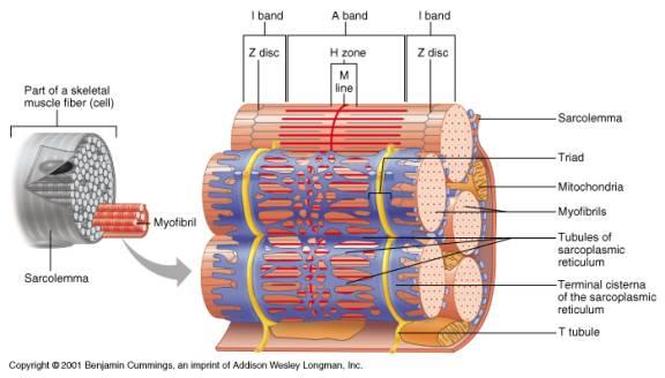
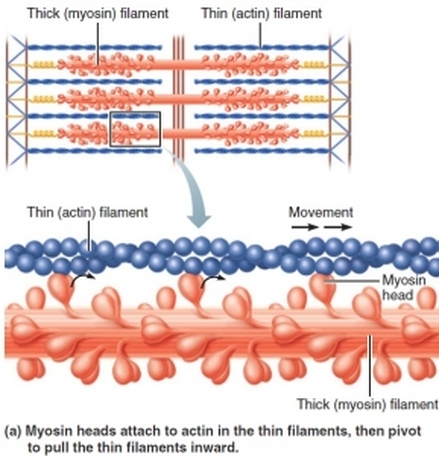
Each skeletal muscle is surrounded by a connective tissue sheath called the epimysium or muscular fascia. A muscle is composed of numerous visible bundles called muscle fasciculi, which are surrounded by loose connective tissue called the perimysium. A fascicles is composed of several muscle cells, which are called muscle fibers. Each muscle fiber is surrounded by loose connective tissue called endomysium. Under the light microscope, the light and dark striations in skeletal muscle fibers are clearly visible. These striations result from the internal structure of long, rod-shaped organelles called myofibrils. Myofibrils are unbranched cylinders that are present in large numbers, making up more than 80% of the sarcoplasm. They are specialized in contractile organelles unique to muscle tissue. The myofibrils in a fiber are separated from one another by other components of a sarcoplasm. Among those components are mitochondria and glycosides, both of which supply energy for muscle contraction. A myofibril is a long row of repeating segments called sacromeres. The sacromere is the basic unit of contraction skeletal muscle. The boundaries at the two ends of each sacromere are called Z discs. Attached to each Z disc and extending toward the center of the sacromere are many fine myofilaments called thin (actin) filaments, which consist primarily of the protein actin, although they contain other proteins as well. In the center of the sacromere and overlapping the inner ends of the thin filaments is a cylindrical bundle of thick (myosin) filaments. Thick filaments consist largely of myosin molecules. THey also contain ATPase enzymes that split ATP to release the energy required for muscle contraction. Both ends of thick filaments are studded with knobs called myosin heads.
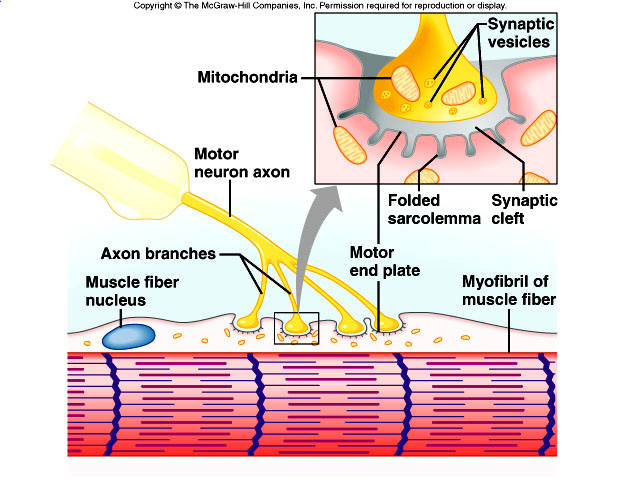
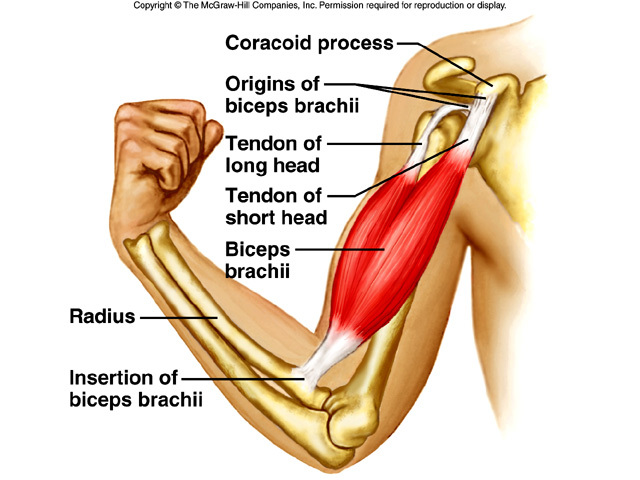
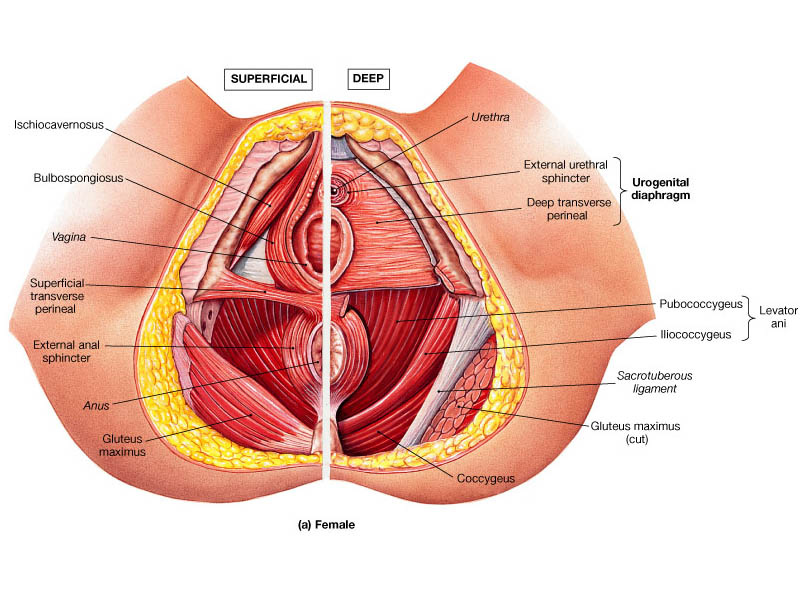
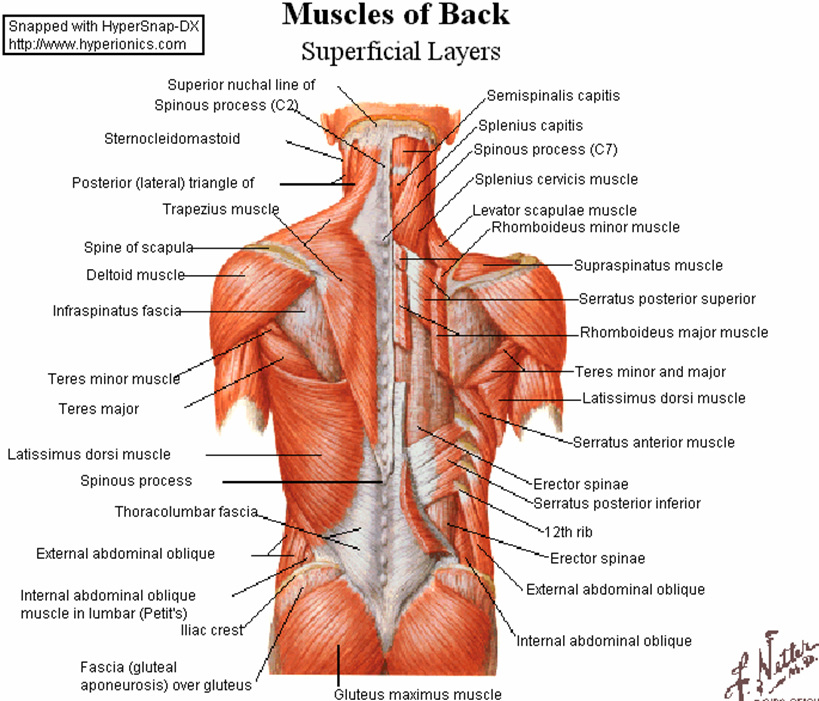
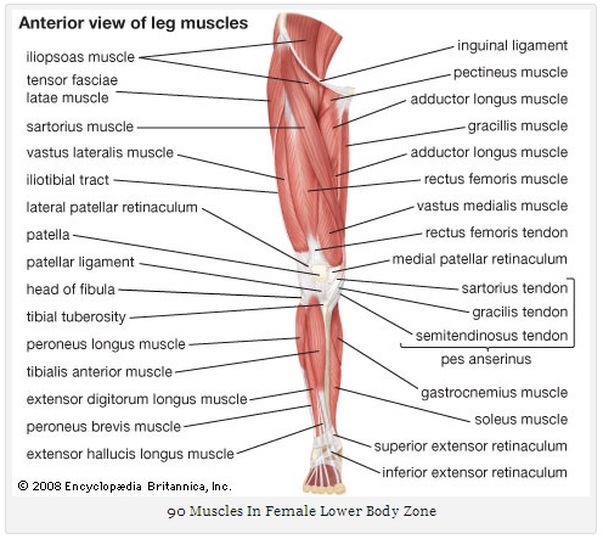
The Sacromere structure explains the pattern of striations in skeletal muscle fibers. The dark bands are created by the full length of the thick filaments in the sacromeres, along with the inner ends of the thin filaments, which overlap the thick filaments. This region of each sacromere, is called the A band. The central part of an A band, where no thin filaments reach, is the H Zone. The M line in the center of the H zone contains tiny rods that hold the thick filaments together. THe two regions on either side of the A band, regions that contain only thin filaments, are called the I bands. It is the I bands of the sacromeres that create the light portions of the light-dark pattern of striations seen along the length of any skeletal muscle fiber. There are two types of muscle contraction involved in producing movement: concentric contraction and eccentric contraction. Concentric contraction is the more familiar type, in which the muscle shortens and does work- picking up a book or kicking a ball. Eccentric contraction- occurs when a muscle generates force as it lengthens. The mechanism for this type of contraction is less understood, but eccentric contractions are essential for controlled movement and resistance to gravity. The release of calcium ions from the sarcoplasmic reticulum and the subsequent contraction of skeletal muscle is initiated by nervous stimulation. THe nerve cells that innervate muscle fibers are called motor neurons. Each muscle fiber in a skeletal muscle is served by a nerve ending, which signals the fiber to contract. The point at which the nerve ending and fiber meet is called a neuromuscular junction. The nerve part of the junction is a cluster of enlargements at the end of the axonal process that stores chemical messenger molecules, neurotransmitters. These enlargements are called axon terminals. The axon terminals are separated from the sarcolemma of the muscle fiber by a space called the synaptic cleft. THe axon terminals contain vesicles that release neurotransmitters when a nerve impulse reaches the terminals. The neurotransmitters at the neuromuscular junction-acetylcholine-diffuses across the synaptic cleft and binds to receptor molecules on the sarcolemma, where it induces an impulse that initiates fiber contraction. The two points of attachment of each muscle are its origin and insertion. The origin, also called the head, is the most stationary end of the muscle. The insertion is the end of the muscle attached to the bone undergoing the greatest movement. Origins are usually, but not always, proximal or medial to the insertion of a given muscle. THe part of the muscle between the origin and the insertion is the belly.
Muscles are typically grouped so that the action of one muscle or group of muscles is opposed by that of another muscle or group of muscles. A muscle that accomplishes a certain movement, such as flexion, is called the agonist. A muscle acting in opposition to an agonist is called an antagonist. Members of a group of muscles working together to produce a movement are called synergists. Among a group of synergists, if one muscle plays the major role in accomplishing the desired movement, it is called the prime mover. Fixators are muscles that hold one bone in place relative to the body while a usually more distal bone is moved.
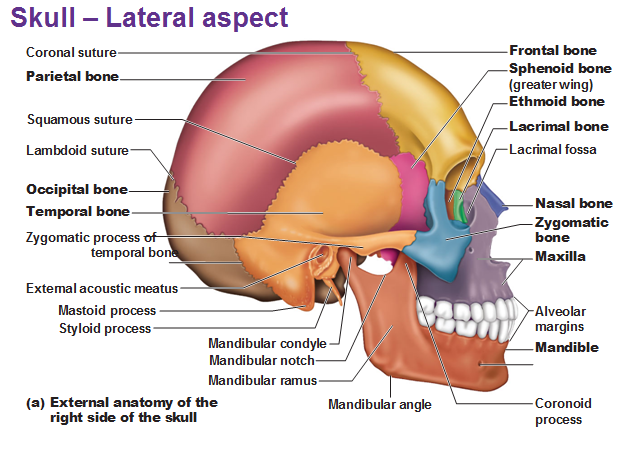
Lateral View of the Skull
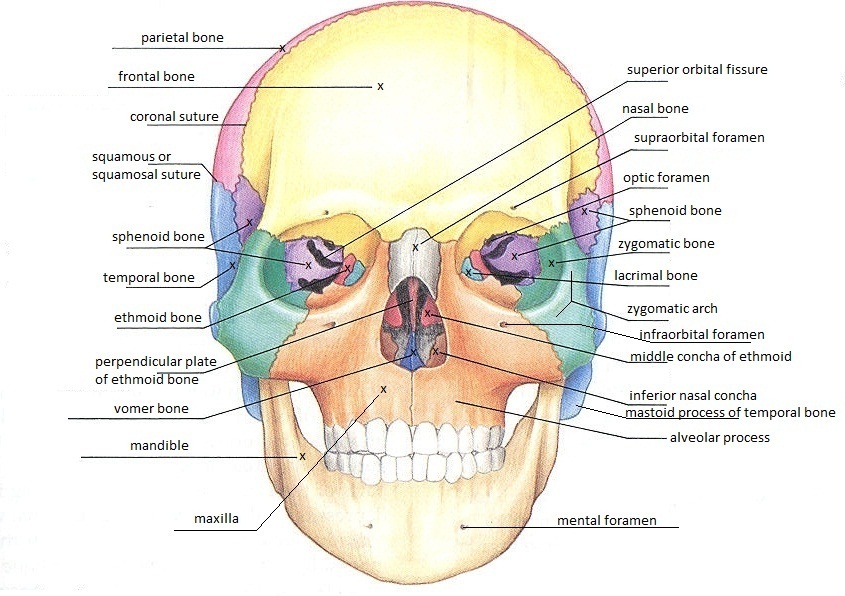
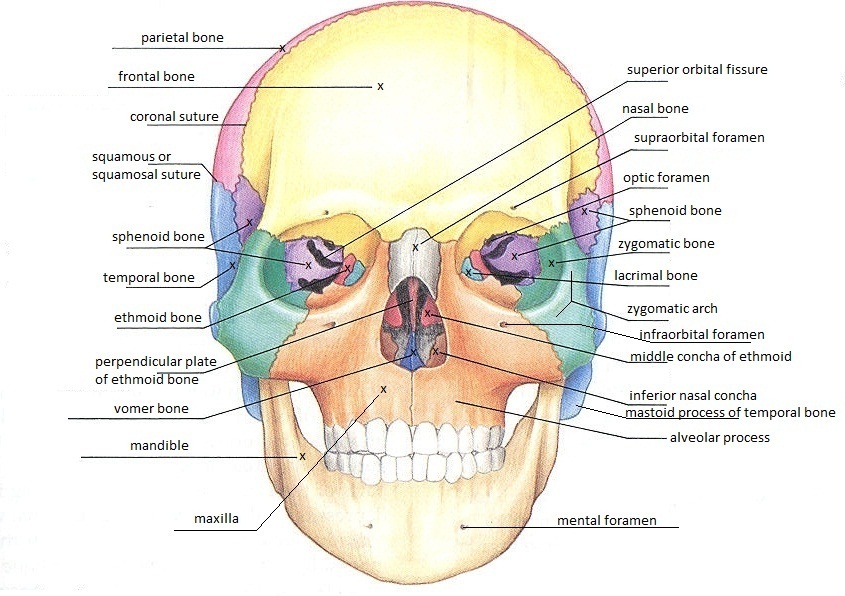
Frontal View of the Skull
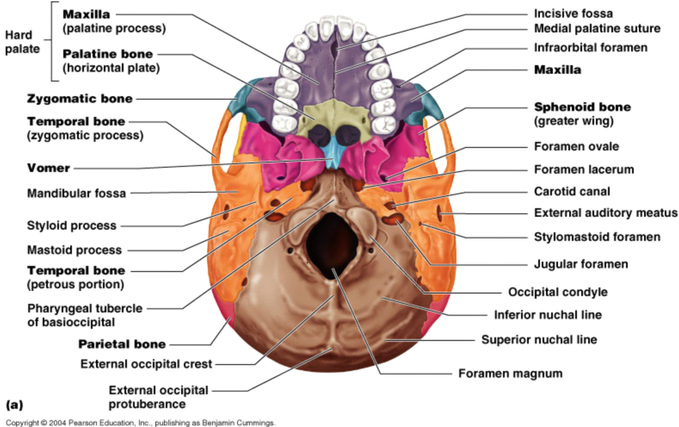
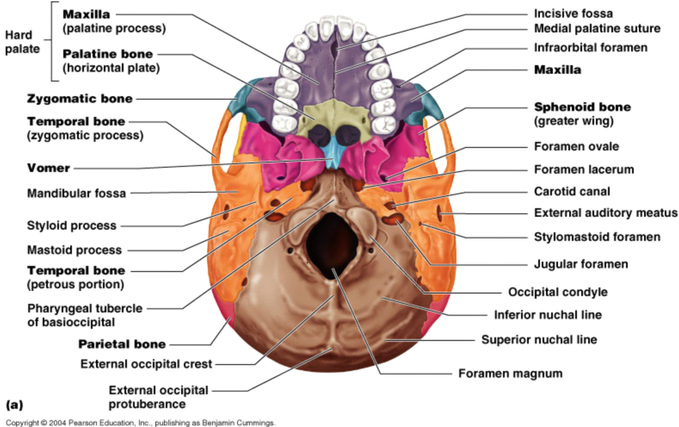
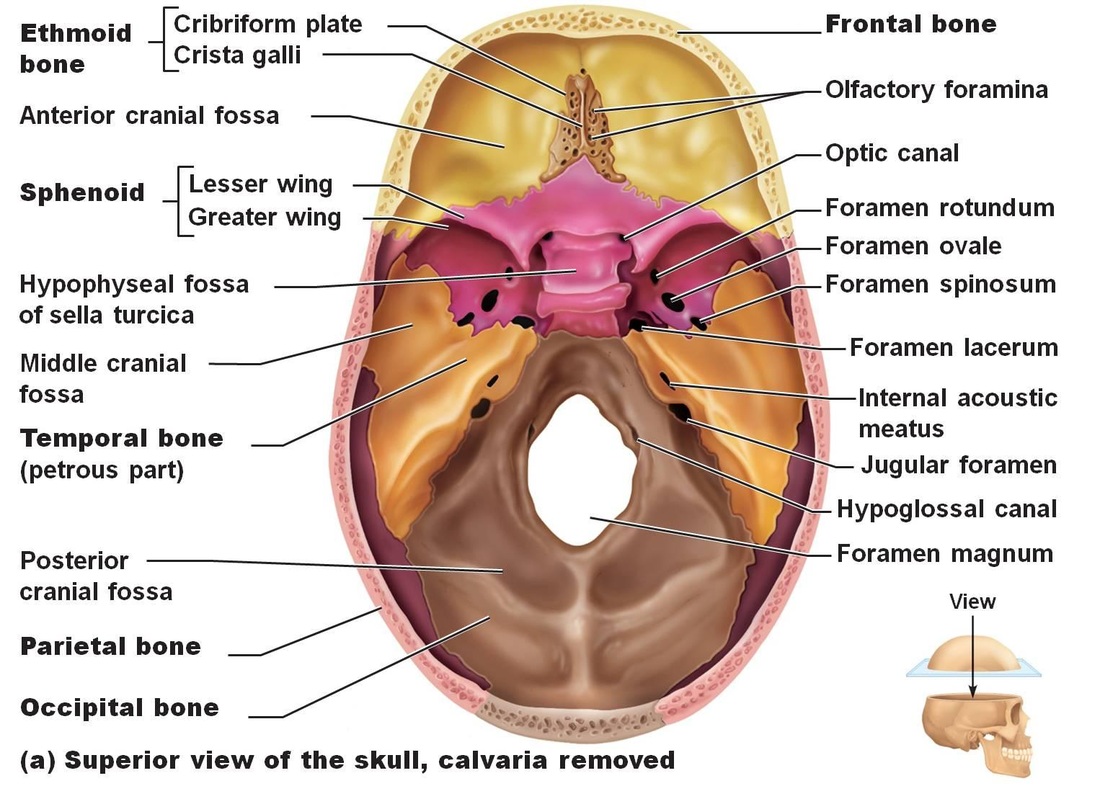
Inferior View of the Skull
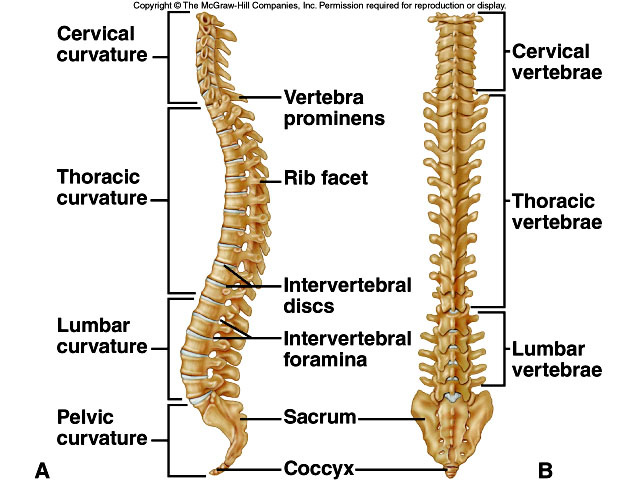
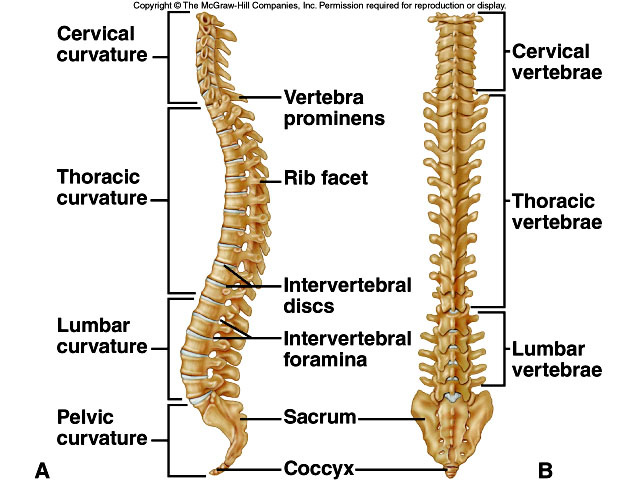
Vertebral Column
Humerus Bone
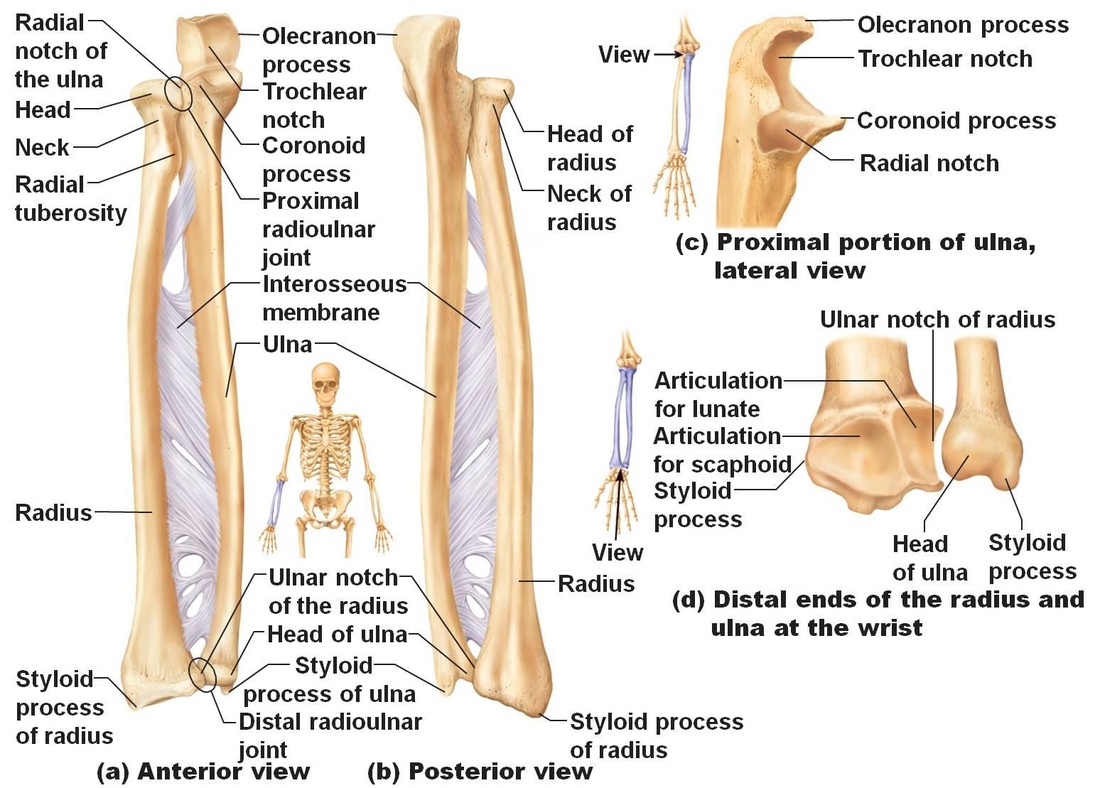
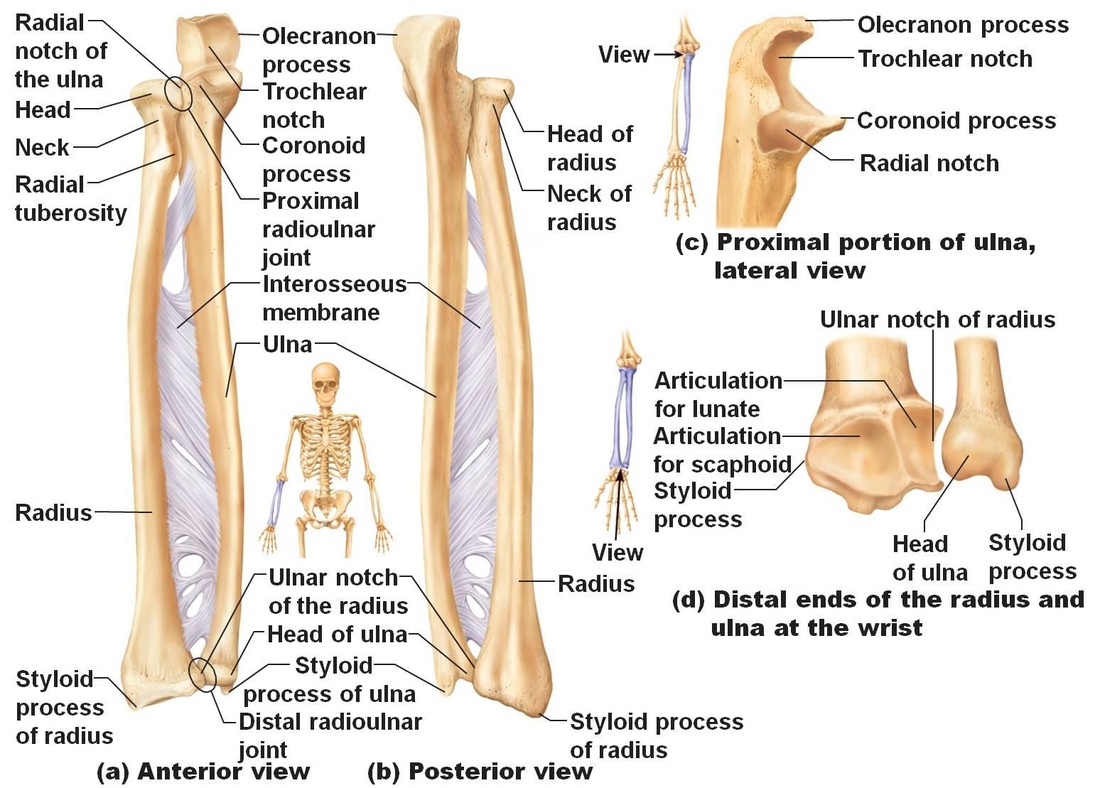
Radius and Ulna
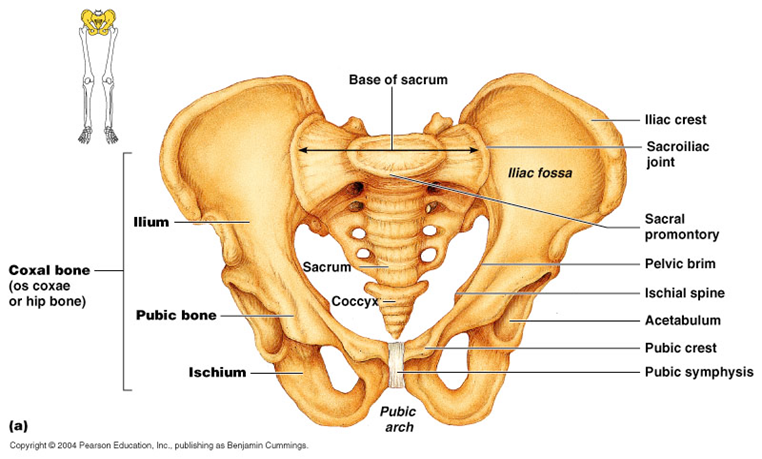
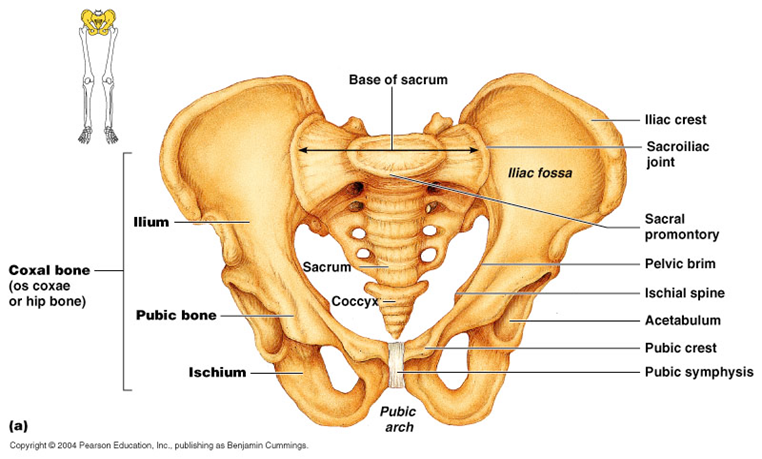
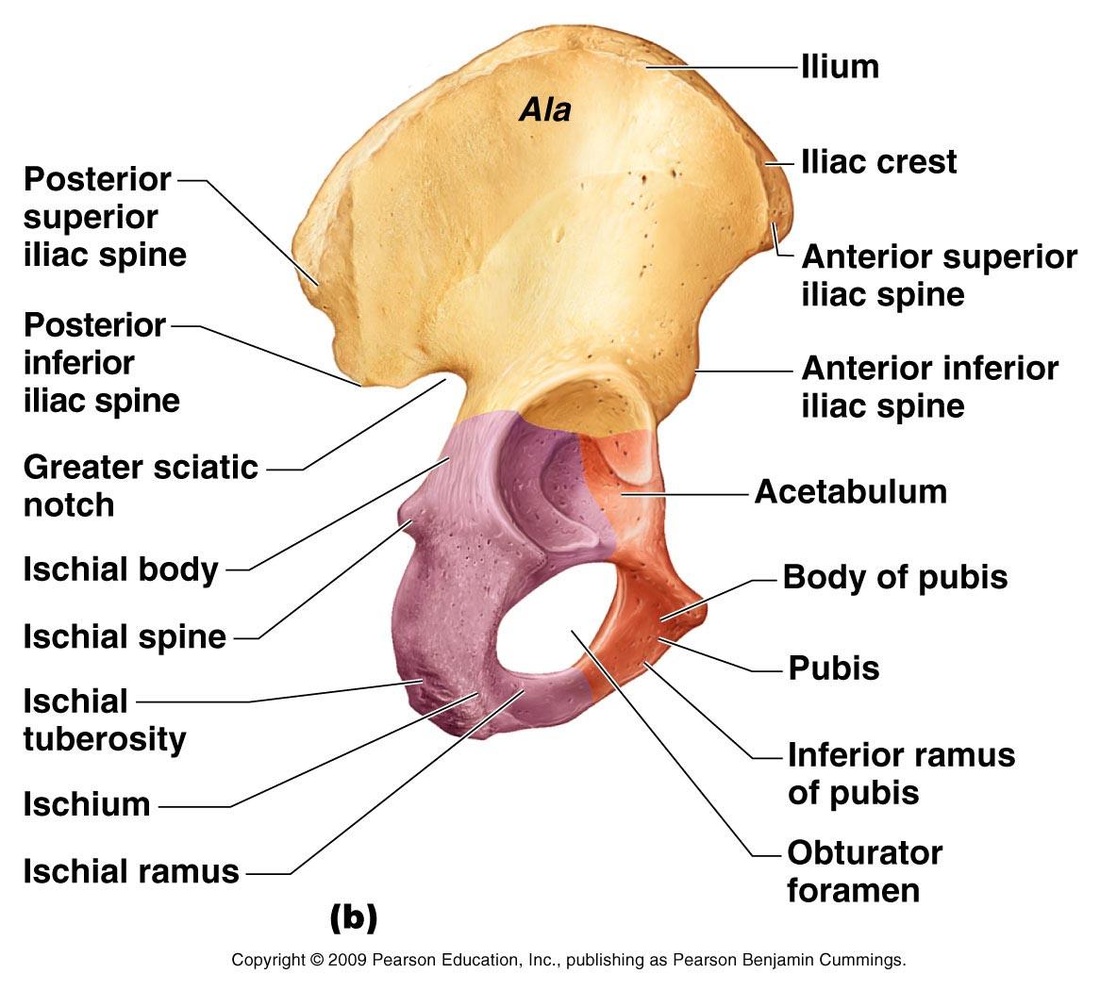
Pelvis
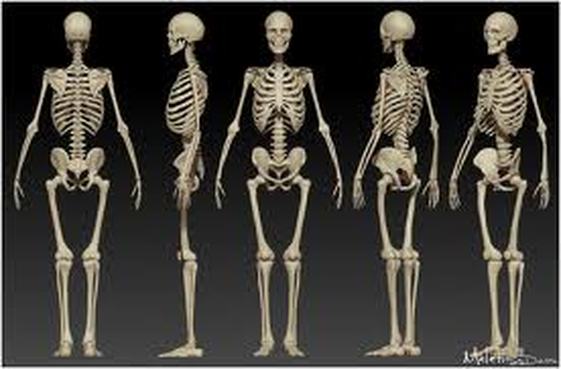
Functions of the Skeletal System:
1. Support
2. Protection
3. Movement
4.Storage
5. Blood cell production
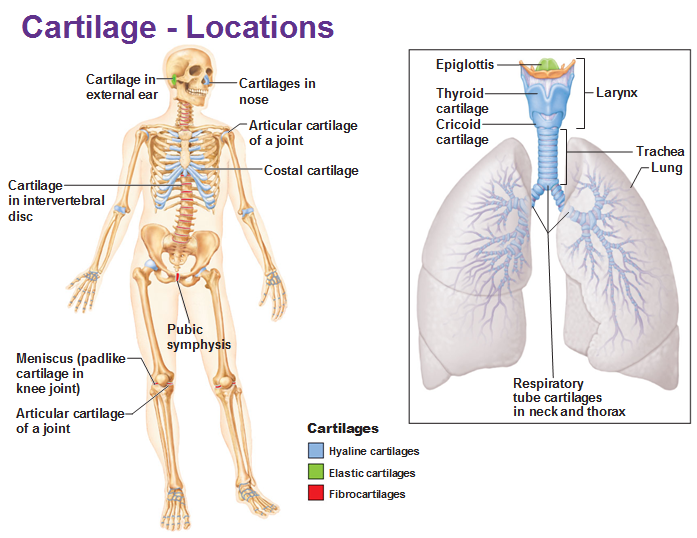
Types of Cartilage: Hyaline cartilage, elastic cartilage, and fibrocartilage.
Hyaline Cartilage: most abundant type of cartilage. The only type of fiber in the matrix is a collagen unit fibril, which forms networks that are too thin to be seen with alight microscope. The gelatinous ground substance holds large amounts of water; thus this tissue resists compression well. Hyaline cartilage proves support through flexibility and resilience.
Elastic Cartilage- its matrix contains many elastic fibers along with the delicate collagen fibrils. This cartilage is more elastic than hyaline and is better able to tolerate repeated bending.
Fibrocartilage- is an unusual tissue that resists both strong compression and strong tension (pulling) forces. It occurs in certain lima gents and certain cartilages that experience both of these forces. 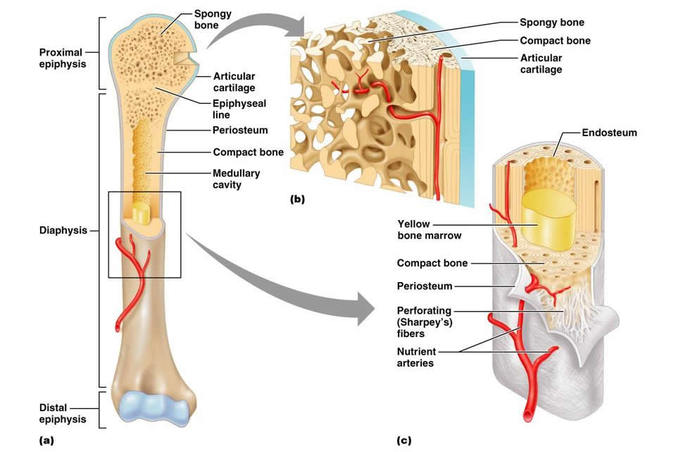 Structure of a long bone Structure of aTypical Long Bone
The tubular diaphysis, or shaft, forms the long axis of a long bone. The epiphysis are the bone ends. The joint surface of each epiphysis is covered with a thin later of hyaline cartilage called the articular cartilage. Between the diaphysis and each epiphysis of an adult long bone is an epiphyseal line. This line is a remnant of the epiphyseal plate, a disc of hyaline cartilage that grows during childhood to lengthen the bone.
The Medullary Cavity- The interior of all bones consists largely of spongy bone. However, the very center of the diaphysis of a long bone contains no bone tissue at all and is called the medullary cavity or marrow cavity. This cavity is filled with yellow bone marrow.
Membranes:
Periosteum- covers the entire outer surface of each bone except on the ends of the epiphysis, where articular cartilage occurs.
Endosteum- covers the internal surfaces of bones. Specifically, endosteum covers the trabecular of spongy bone; it also lines the central canals of osteons.
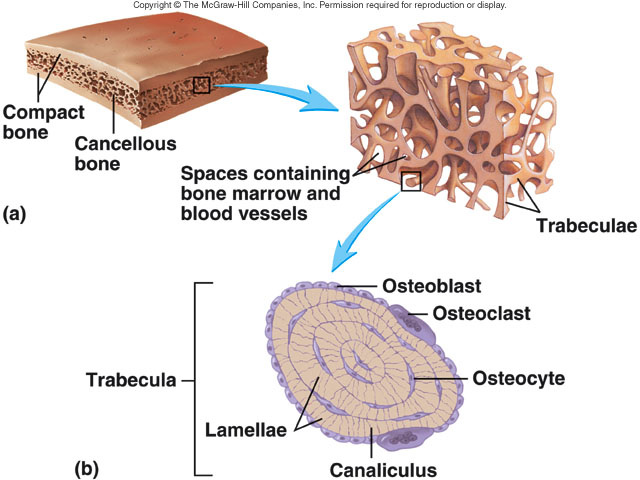
Almost every bone of the skeleton has a dense outer layer that looks smooth and solid to the naked eye. This eternal layer is compact bone. Internal to this is spongy bone also called trabecular bone, a honeycomb of small needle-like or flat pieces called trabeculae. In this network, the open spas between the trabecular are filled with red or yellow bone marrow.
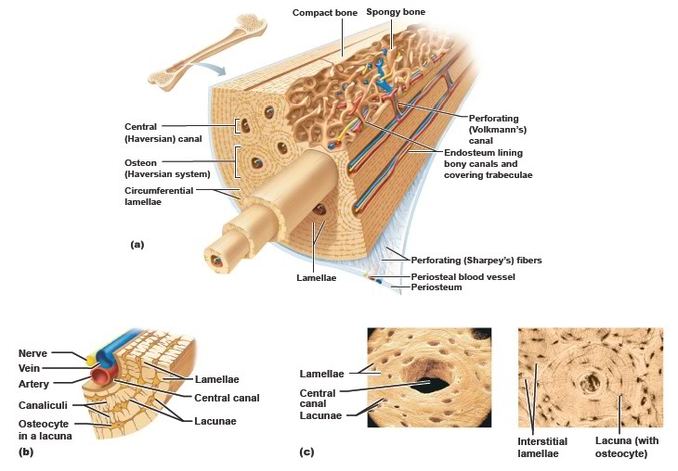
Short, irregular, and flat bones have much the same composition as long bones: the periosteum-covered compact bone externally and endosteum-covered spongy bone internally. However, because these bones are not cylindrical, they have no diaphysis. They contain bone marrow (between the trabecular of their spongy bone), but no marrow cavity is present. In flat bones, the internal spongy bone is called diploe. 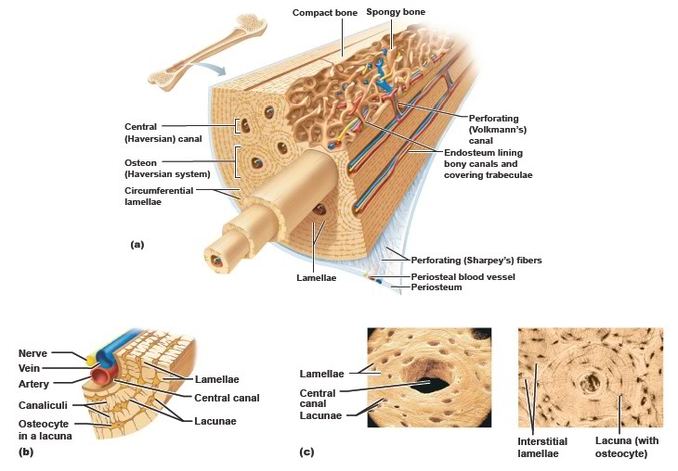 Microscopic Structure of compact bone An important structural component of compact bone is the osteon or Haversion System. Osteons are long, cylindrical structures oriented parallel to the long axis of the bone and to the main compression stresses. Functionally, osteons can be viewed as miniature weight-bearing pillars. Structurally, an osteon is a group of concentric tubes resembling the rings of tree trunk in cross section. Each of the tubes is a lamella, a layer of bone matrix in which the collagen fibers and mineral crystals align and run in a single direction.
Through the core of each osteon runs a canal called the central canal or Haversian canal. Like all internal bone cavities, it is lined by endosteum. The central canal contains its own blood vessels, which supply nutrients to the bone cells of the osteon, and its own nerve fibers.
Perforating canals also called Volkmann's canals, lie at right angles to the central canals and connect the blood and nerve supply of the periosteum to that of the central canals and the marrow cavity.
The mature bone cells, the osteocytes, are spider-shaped. Their bodies occupy small cavities in the solid matrix called lacunae, and their legs occupy thin tubes called canaliculi. These "little canals" run through the matrix, connecting neighboring lacunae to one another and to the nearest capillaries, such as those in the central canals.
Lying in between lamellae in compact bone are groups of incomplete lamellae called interstitial lamellae. These are simply the remains of old osteons that have been cut through by bone remodeling. Additionally, circumferential lamellae occur in the external and internal surfaces of the layer of compact bone; each of these lamellae extends around the entire circumference of the diaphysis. The circumferential lamellae effectively resist twisting of the entire long bone.
Bone Development and Growth
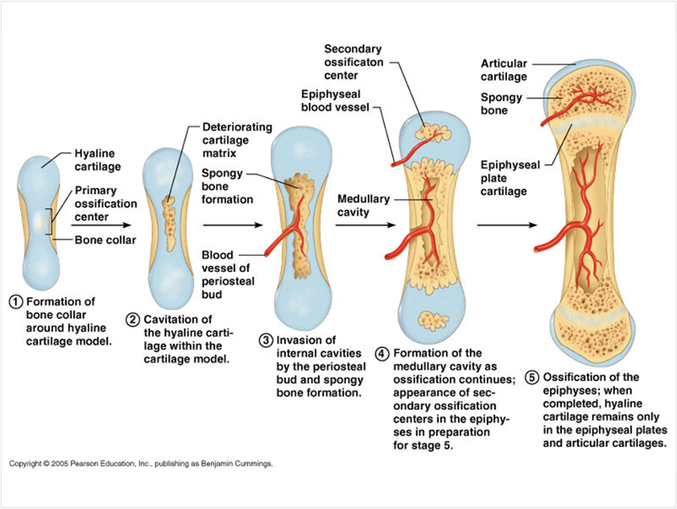
Osteogenesis and ossification are both names for the process of bone-tissue formation. Osteogenesis begins in the embryo, proceeds through childhood and adolescence as the skeleton grows, and then occurs at a slower rate in the adult as part of a continual remodeling of the full-grown skeleton.
Before week 8, the skeleton of the human embryo consists only of hyaline cartilage and some membranes of mesenchyme, and embryonic connective tissue. Bone tissue first appears in week 8 and eventually replaces most cartilage and mesenchymal membranes in the skeleton. Some bones, called membrane bones, develop from a mesenchymal membrane through a process called intramembranous ossification. Other bones develop as hyaline cartilage, which is replaced through a process called endochondral ossification. These bones are called endochondral bones or cartilage replacement bones. 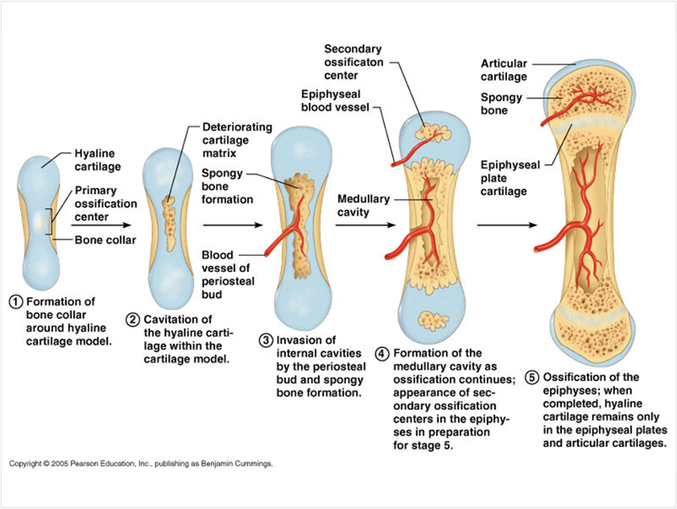 Endochondral Ossification of a long bone Repair of Bone Fractures
Despite their strength, bones are susceptible to fractures, or breaks. A fracture in which the bone breaks cleanly but does not penetrate the skin is a simple fracture. When broken ends of the bone protrude through the skin, the fracture is compound. A fracture is treated by reduction, realignment of the broken bone ends. In closed reduction, the bone ends are coaxed back into position by the physician's hands. In open reduction, the bone ends are joined surgically with pins or wires. After the broken bone is reduced, it is immobilized by a cast or traction to allow the healing process to begin. Healing time is about 6 to 8 weeks for a simple fracture, but it is longer for large, weight-bearing bones and for the bones of older people. 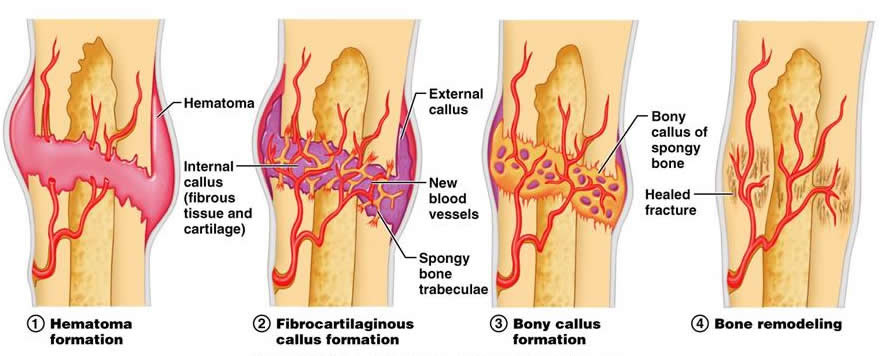 Stages in the healing of a bone fracture - Hematoma Formation. The fracture is usually accompanied by hemorrhaging. Blood vessels break in the periosteum and inside the bone, releasing blood that clots to form a hematoma.
- Fibrocartilaginous callus formation. WIthin a few days, new blood vessels grow into the clot. The periosteum and endosteum near the fracture site show a proliferation of bone-forming cells, which then invade the clot, filling it with repair tissue called soft callus. As fibers are produced, the soft callus becomes a dense connective tissue containing fibrocartilage and hyaline cartilage.
- Bony callus formation. within a week, the trabecular of new bone begins to form in the callus, mostly by endochondral ossification. These trabecular span the width of the callus and unite the two fragments of the broken bone. The callus is not called a bony callus or hard callus and its trabeculae grow thicker and stronger and become firm about 2 months after the injury.
- Bone remodeling. Over a period of many months, the bony callus is remodeled. The excess body material is removed from both the exterior of the bone shaft and the interior of the medullary cavity. Compact bone is laid down to reconstruct the shaft walls. The repaired area resembles the original unbroken bone region, because it responds to the same set of mechanical stresses.
The Integumentary System consists of the hair, nails, and skin. Integument means covering, and the integumentary system covers the outside of the body.
Functions of the Integumentary System: Protection, Sensation, Vitamin D production, Temperature Regulation, and Excretion.
The Skin
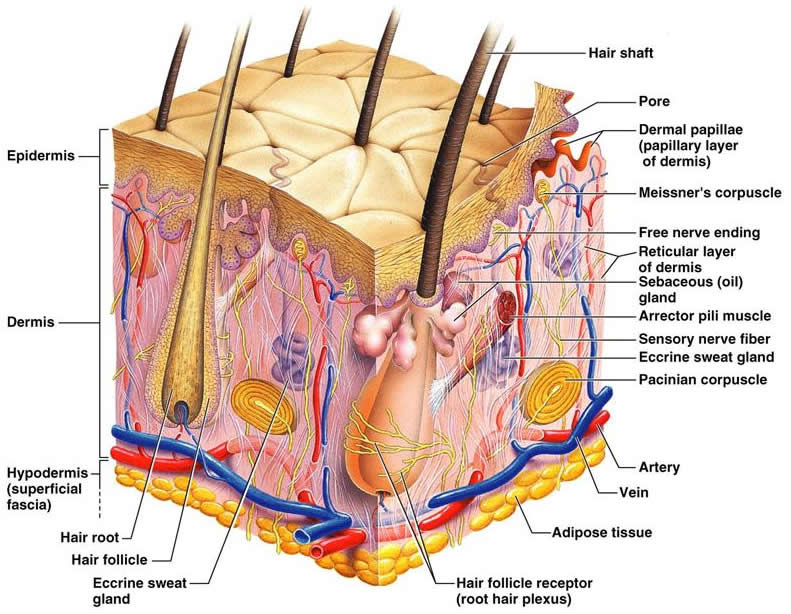
The Skin is made up of two major tissue layers. The Epidermis is the most superficial layer of the skin. It is a layer of epithelial tissue that rests on the dermis, a layer of dense connective tissue. The epidermis prevents water loss and resists abrasion. The dermis is responsible for most of the skin's structural strength. The skin rests on the subcutaneous tissue, which is a layer of connective tissue. The subcutaneous tissue is not part of the skin, but it does connect the skin to underlying muscle or bone. 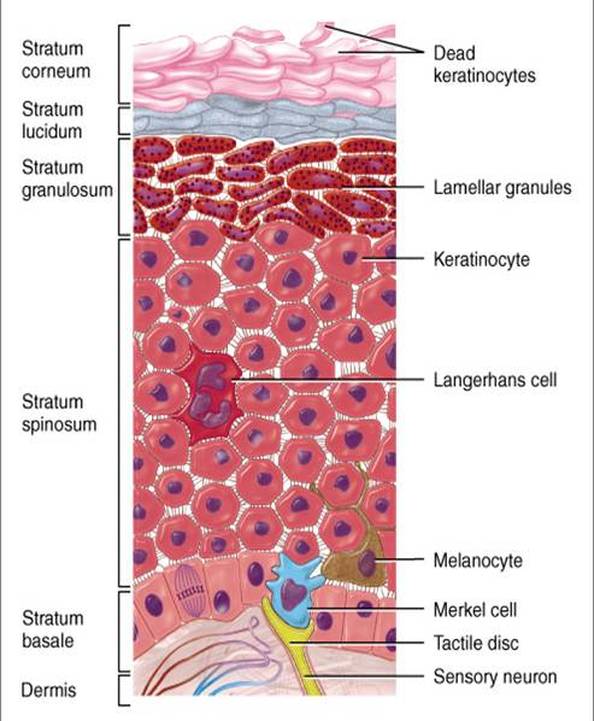
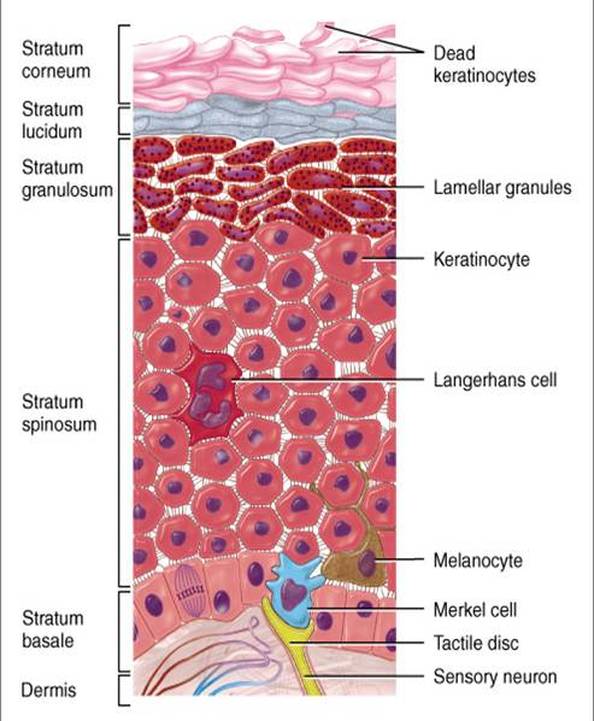
The Epidermis is a keratinized stratified squamous epithelium that contains four distinct types of cells: keratinocytes, melanocytes, tactile epithelial cells, and dendritic cells. Keratinocytes, the most abundant epidermal cell, produce keratin, a tough fibrous protein that gives the epidermis its protective properties. Keratinocytes also produce produce antibiotics and enzymes that detoxify the harmful chemicals to which our skin is exposed. Keratinocytes arise in the deepest part of the epidermis from cells that undergo almost continuous mitosis. As these cells are pushed up by the production of new cells beneath them, they make the keratin that eventually fills their cytoplasm. By the time they approach the skin surface, they are dead, flat sacs completely filled with keratin.
Layers of the Epidermis:
Stratum Basale- deepest epidermal layer, firmly attached to the underlying dermis along a wavy borderline. It consists of a single row of cells, mostly stem cells representing the youngest keratinocytes. These cells divide rapidly, and many mitotic nuclei are visible. Tactile epithelial cells or merkel cells are distributed sparsely among the keratinocytes. Each tactile epithelial cell is intimately associated with a dislike sensory nerve ending and functions as a receptor for touch. About 10%-25% of the cells in the stratum basal are melanocytes, which make the dark skin pigment melanin.
Stratum Spinosum- is several layers thick. Cells of the stratum spinosum consist of a tension-resisting protein pre-keratin. Scattered among the keratinocytes of the stratum spinosum are dendritic cells. Dendritic cells police the outer body surface, using receptor-mediated endocytosis to take up foreign proteins (antigens) that have invaded the epidermis.
Stratum Granulosum- consists of one to five layers of flattened keratinocytes. Along with abundant pre-keratin intermediate filaments, these cells also contain keratohyalin granules and lamellated granules. The keratohyalin granules help form keratin in the more superficial layers. The lamellated granules contain a waterproofing glycolipid that is secreted into the extracellular space and plays a major role in slowing water loss across the epidermis. Furthermore, the plasma membranes of the cells thicken so that they become more resistant to destruction.
Stratum Lucidum- occurs in thick skin. Consists of a few rows of flat, dead keratinocytes.
Stratum Corneum- The most external part of the epidermis, consists of many layers of cells. Its dead keratinocytes are flat sacs completely filled with keratin because their nuclei and organelles disintegrated upon cell death. Keratin consists of the pre-keratin intermediate filament embedded in a "glue" from the keratohyalin granules. Both the keratin and the thickened plasma membranes of cells in the stratum corneum protect the skin against abrasion and penetration. Additionally, the glycolipid between its cells keep this later waterproof.
Layers of the Dermis
The Dermis, is a strong, flexible connective tissue. The cells of the dermis are typical of any connective tissue proper: fibroblasts, macrophages, mast cells, and scattered white blood cells. The fibers are: collagen, elastic, and reticular.
The Dermis is richly supplied with nerve fibers and blood vessels. The dermal blood vessels consist of two vascular plexuses (a plexus is a network of converging and diverging vessels). The deep dermal plexus is located between the hypodermic and the dermis. It nourishes the hypodermic and the structures located within the deeper portions of the dermis. The more superficial sub papillary plexus, located just below the dermal papillae, supplies the more superficial dermal structures, the dermal papillae, and the epidermis. Dermal blood vessels do more than just nourish the dermis and overlying epidermis; they also perform a critical role in temperature regulation.
The dermis has two layers: papillary and reticular. The papillary layer, the superficial 20% of the dermis, is areolar connective tissue containing very thin collagen and elastic fibers. It includes the dermal papillae, finger-like projections that extend into the overlying epidermis. These projections of the dermal papillae into the epidermis increase the surface area for exchange of gases, nutrients, and waste products between these laters. The deeper reticular layer, which accounts for about 80% of the thickness of the dermis, is dense irregular connective tissue. Its extracellular matrix contains thick bundles of interlacing collagen and elastic fibers that run in many different planes. The reticular layer is named for its networks of collagen fibers; the name does not imply any special abundance of reticular fibers. Separations or less dense regions between the collagen bundles form the cleavage lines or tension lines of the skin. The Hypodermis also called the superficial fascia and subcutaneous layer consists of both areolar and adipose connective tissue, but adipose tissue normally predominates. Besides storing fat, the hypodermic anchors the skin to the underlined structures, but loosely enough that the skin can slide relatively freely over those structures.
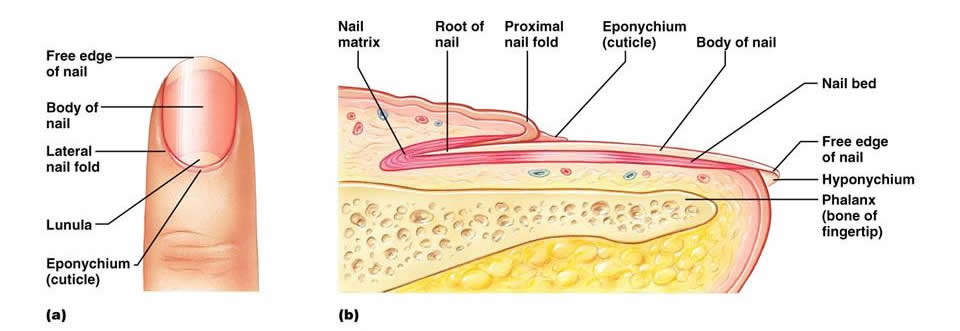
The Nails
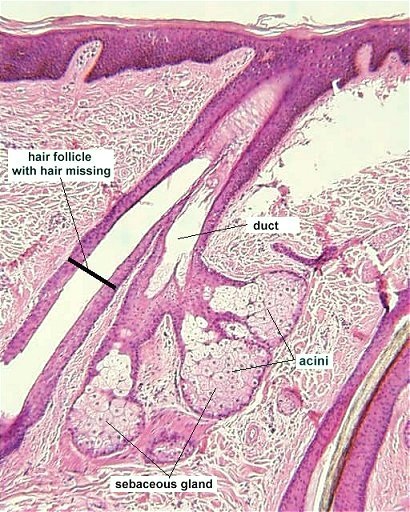
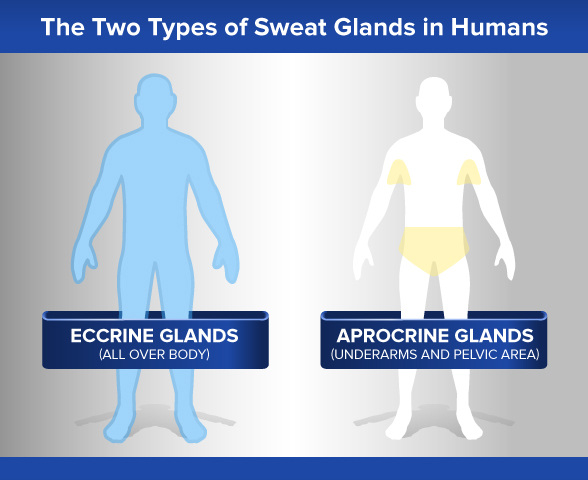
Nails are made of dead, keratinized cells. The hard keratin that predominates in hairs and nails differs from the soft keratin that is found in typical epidermal cells. Each nail has a distal free edge, a body (the visible attached part) and a root (the proximal part embedded in the skin). The nail rests on a bed of epidermis called the nail bed. Hair is a flexible strand made of dead cells filled with card keratin. The chief parts of hair are the root, the part embedded in the skin, and the shaft, the part that projects above the skin surface. A hair consists of three concentric laters of keratinized cells. Its central core, the medulla, consists of large cells and air spaces. The medulla is absent in fine hairs. The cortex, surrounding the medulla, consists of several layers of flattened cells. The outermost cuticle is a single later of cells that overlap one another from below like shingles on a roof. This shingle pattern helps to keep neighboring hairs apart so that the hair does not mat. Sebaceous Glands are the skin's oil glands. They are simple alveolar glands with several alveoli opening into a single duct, but the alveoli are actually filled with cells, so there is no lumen (central cavity). THeir oily product is called sebum. There are two types of sweat glands: Eccrine glands and Apocrine glands.
Eccrine glands are by far the more numerous type and produce true sweat. They are most abundant on the palms, soles, and forehead. Each is a coiled version of a simple tubular gland. The coiled, secretory base lies in the deep dermis and hypodermic, and the fact runs superficially to open at the skin surface through a funnel shaped pore.
Apocrine glands are mostly confined to the axillary, anal, and genital areas. They are larger than eccrine glands and produce a special kind of sweat consisting of fatty substances and proteins, in addition to the components of true sweat. For this reason, apocrine sweat is viscous and sometimes has a milky or yellow color. THis product is odorless when first secreted, but its organic molecules are decomposed by bacteria on the skin, it takes on a musky smell. This is the source of body odor.
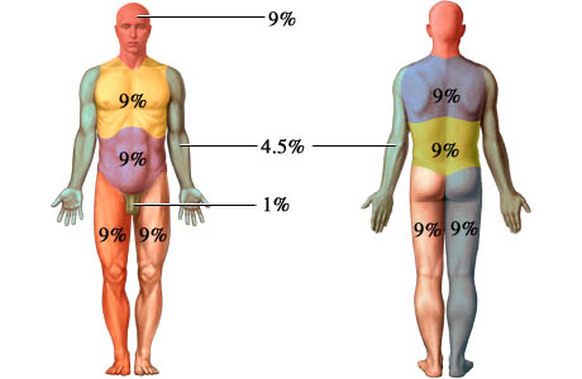
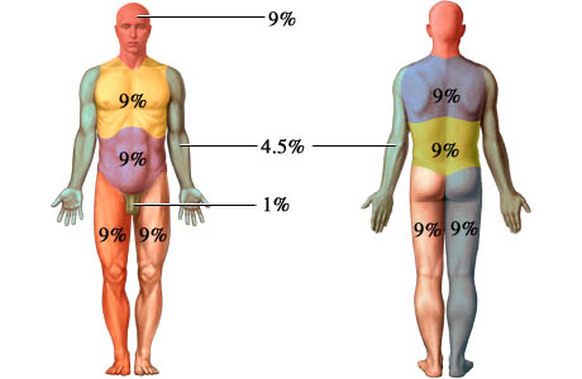
Burns ; Rule of Nines- Used to estimate extent of burns
Burns are classified by their severity as first-, second-, or third-degree burns.
First-degree burns- Only the epidermis is damaged. Symptoms include redness, swelling, and pain: the typical inflammatory reaction to tissue damage. Generally first-degree burns heal in a few days without special attention.
Second-degree burns- involve injury to the epidermis and the upper part of the dermis. Symptoms resemble those of first-degree burns, but blisters also appear as fluid accumulates between the epidermal and dermal layers. The skin regenerates with little or no scarring in 3 to 4 weeks if care is taken to prevent infection. First-and second-degree burns are considered partial-thickness burns.
Third-Degree burns- consume the entire thickness of the skin, and thus are full-thickness burns. The burned area appears white, red, or blackened. Although the skin might eventually regenerate, it is usually impossible to wait for this because of fluid loss and infection. Therefore skin from other parts of the patient's body must be grafted onto the burned area.

Skin Cancer: Melanoma
Skin cancer is the most common type of cancer, with about a million new cases appearing each year in the United States.
Melanoma- a cancer of melanocytes, is the most dangerous type of skin cancer. Melanocytes are derived from neural crest cells, which wander widely during embryonic development. This predisposition for migration may explain the invasive nature of melanoma. Melanoma accounts for only about 1 out of every 20 skin cancers, but it is increasing rapidly in countries with light-skinned populations- by 3% to 8% per year in the United States. Melanoma can originate wherever there is pigment, but it often arises from existing moles, usually appearing as an expanded dark patch. Because melanoma cells metastasis rapidly into surrounding circulatory vessels, the key to surviving melanoma is early detection. Most people do not survie this cancer if the lesion has grown over 4mm thick. Melanoma is resistant to chemotherapy and current immunotherapy treatment, although vaccines are being tested.
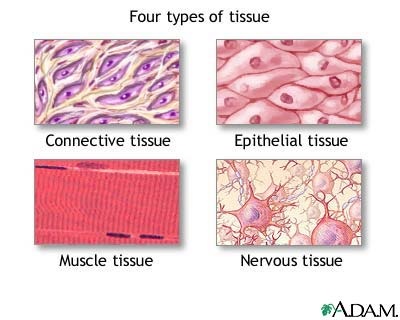
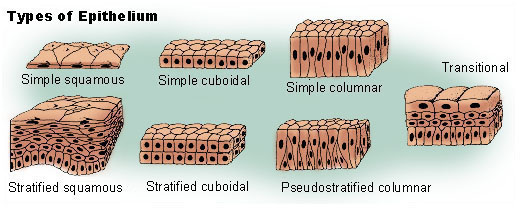
A tissue is a group of cells with similar structure and function that have similar extracellular substances located between them. The microscopic study of tissue structure is called histology. The four basic tissue types are epithelial, connective, muscle, and nervous. Epithelial Tissue. Epithelial tissue (covering or lining), covers external and internal surfaces throughout the body. Surfaces of the body include the outer layer of the skin and the lining of cavities, such as the digestive tract, respiratory passages, and blood vessels. It also forms most glands. Epithelium consists almost entirely of cells with very little extracellular space between them. Although there are some exceptions, most epithelia have a free surface, which is not in contact with other cells, and a basal surface adjacent to a basement membrane, which attaches the epithelial cells to underlying tissues.
Functions of the epithelia are: protecting underlying structures, acting as a barrier, permitting the passage of substances, secreting substances, and absorbing substances. Epithelia are classified according to the number of cell laters and the shape of the cells.
Number of Layers Cell Shape
Simple (one layer) Squamous
Cuboidal
Columnar
Pseudostratified (a modified form of simple epithelium) Columnar
-------------------------------------------------------------
Stratified (more than one layer) Squamous
Cuboidal
Columnar
Transitional (a type of stratified epithelium) 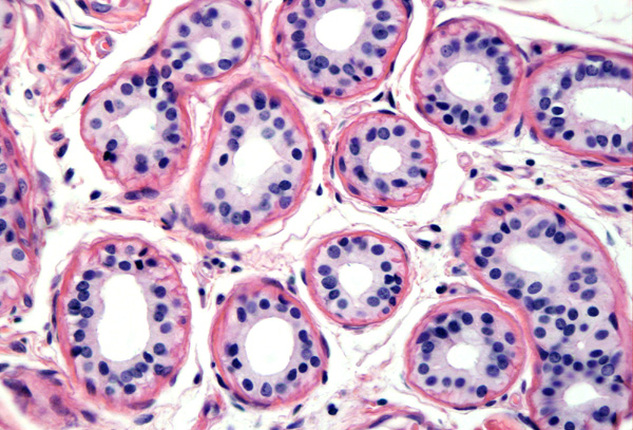
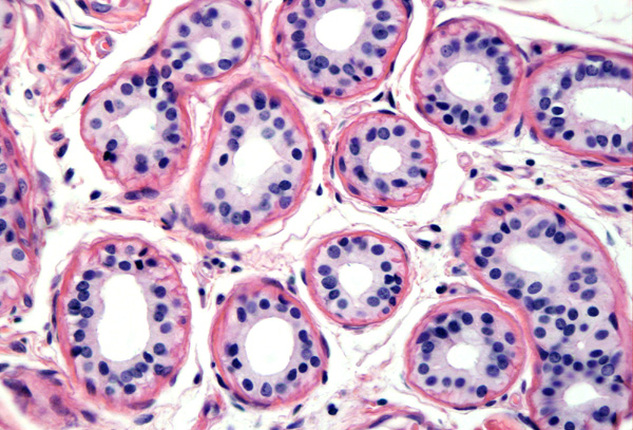
Simple Cuboidal Epithelium.
Function: Active transport and facilitated diffusion result in secretion and absorption by cells of the kidney tubules; secretion by cells of glands and choroid plexuses; movement of particles embedded in mucus out of the terminal bronchioles by ciliated cells.
Location: Kidney tubules, glands and their ducts, choroid plexuses of the brain, lining of terminal bronchioles of the lungs, and surfaces of the ovaries.
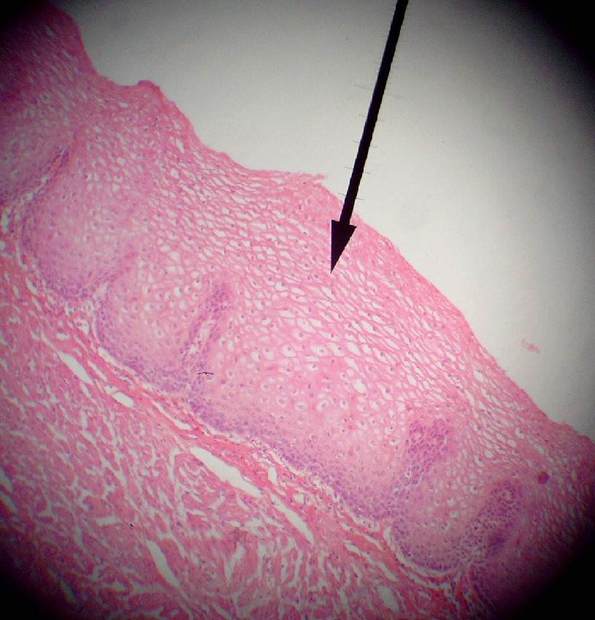
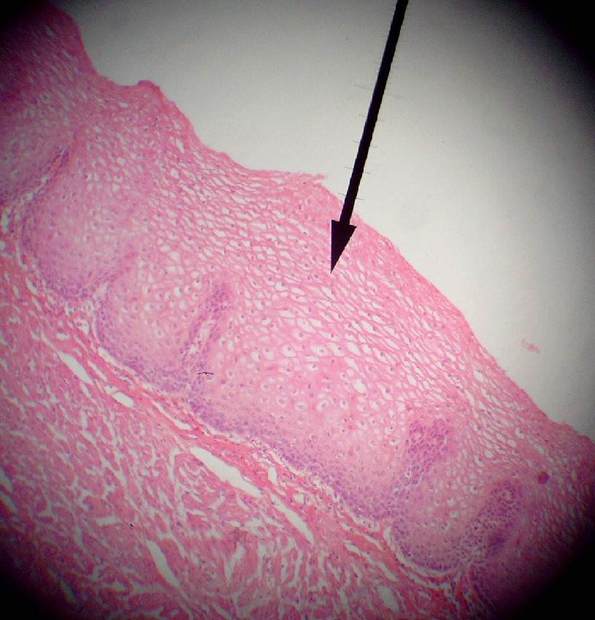
Stratified Squamous Epithelium (non-keratinized)
Function: Protects against abrasion, forms a barrier against infection, and reduces loss of water from the body.
Location: Keratinized - outer later of the skin; Non-Keratinized- mouth, throat, larynx, esophagus, anus, vagina, inferior urethra, and corneas.
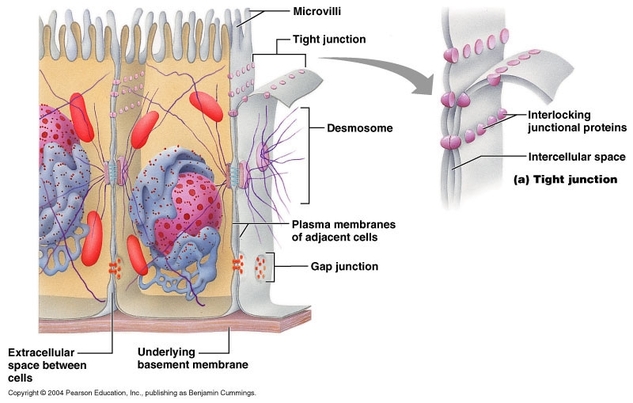 Cell Connections Cell Connections
Epithelial cells are connected to one another in several ways.
Tight Junctions- bind adjacent cells together and form permeability barriers. Tight junctions prevent the passage of materials between epithelial cells because they completely surround each cell, similar to the way a belt surrounds the waist. Materials that pass throughout he epithelial later must pass through the cells, so those cells regulate what materials can cross. Tight junctions are found in the lining of the intestines and in most other simple epithelia.
Desmosomes- mechanical links that bind cells together. Modified desmosomes, called hemidesmosomes also anchor cells to the basement membrane. Many desmosomes are found in epithelia subjected to stress, such as the stratified squamous epithelium of the skin.
Gap Junctions- Small channels that allow small molecules and ions to pass from one epithelial cell to an adjacent one. Most epithelial cells are connected to one another by gap junctions, and researchers believe that molecules or ions moving through the gap junctions act as communication signals to coordinate the activities of the cells.
 Glands Glands
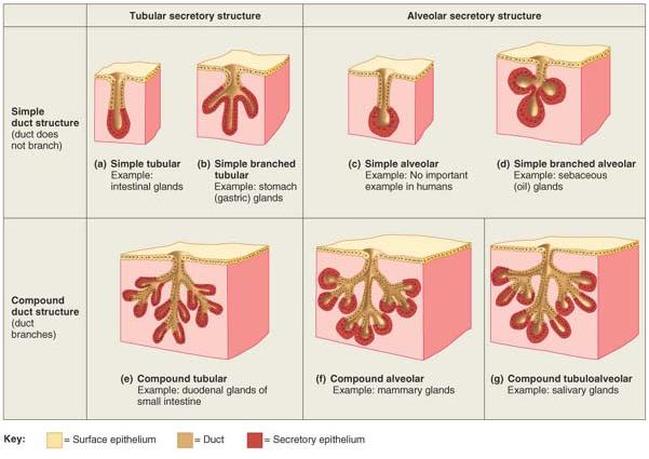
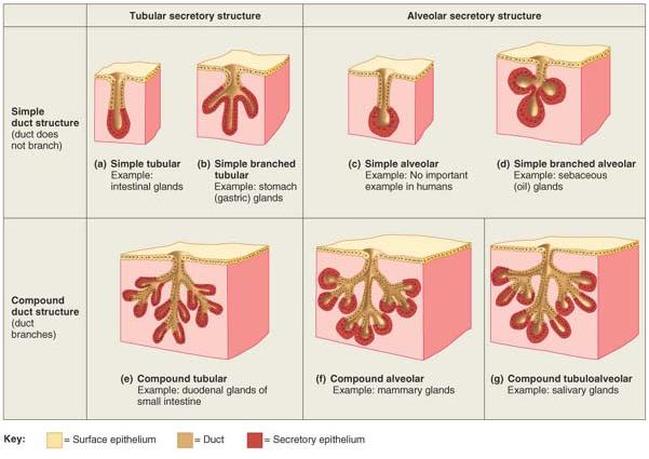
A gland is a structure that secretes substances onto a surface, into a cavity or into the blood. Most glands are composed primarily of epithelium and are multicellular. Glands are classified as endocrine (internal secretions) or exocrine (external secretions), depending on where they secrete their product, and as unicellular ("one-celled") or multicellular ("many-celled") on the basis of cell number.
Endocrine Glands- Lack ducts, so they are often referred to as ductless glands. They secrete directly into the tissue fluid that surrounds them. More specifically, endocrine glands produce messenger molecules called hormones, which they release into the extracellular space. These hormones then enter nearby capillaries and travel through the bloodstream to specific target organs, which are commonly far removed from the endocrine gland that produces the hormone.
Exocrine Glands- All exocrine glands secrete their products onto body surfaces or into body cavities, and multicellular exocrine glands have ducts that carry their product to the epithelial surfaces. The activity of an exocrine gland is local, that is, the secretion acts near the area where it is released.
Unicellular Exocrine Glands- The only important example of a one-celled exocrine gland is the goblet cell. The goblet cells are scattered within the epithelial lining of the intestines and respiratory tubes, between columnar cells with other functions. They produce mucin, a glycoprotein (sugar protein) that dissolves in water when secreted. The resulting complex of mucin and water is mucus. Mucus covers, protects, and lubricates many internal body surfaces.
Multicellular Exocrine Glands- Each multicellular exocrine gland has two basic parts: an epithelium-walled duct and a secretory unit consisting of the secretory epithelium. Multicellular glands are classified by the structure of their ducts. Simple glands have unbranched ducts, whereas compound glands have a branched duct. The glands are further categorized by their secretory units: they are tubular if their secretory cells form tubes and alveolar if the secretory cells form spherical sacs. Furthermore, some glands are tubuloalveolar; that is, they contain both tubular and alveolar units.
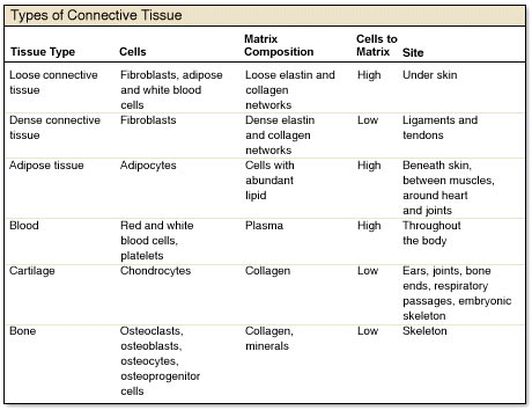
Connective Tissue- The most diverse and abundant type of tissue. There are four main classes of connective tissue and many subclasses. The main classes are: 1.) connective tissue proper 2.) cartilage 3.)bone tissue 4.) blood. Connective tissue do far more than just connect the tissues and organs of the body together. They also form the basis of the skeleton (bone and cartilage), store and carry nutrients (fat tissue and blood), surround all the blood vessels and nerves of the body (connective tissue proper), and lead the body's fight against infection.
Special Characteristics of Connective Tissue: relatively few cells, lots of extracellular matrix, extracellular matrix is composed of ground substance and fibers, embryonic origin.
Cells of the Connective Tissue: In most connective tissues, the primary cell type produces the extracellular matrix. In connective tissue proper, these cells are called fibroblasts. Fibroblasts make the protein subunits of fiber, which then assemble into fibers when the fibroblast secretes them. Fibroblasts also secrete the molecules that form the ground substance of the matrix. In cartilage tissue, the cells that secrete the matrix are called chondroblasts, and in bones they are osteoblasts. Once these tissue-forming cells are not actively secreting new matrix, they are termed fibrocytes, chondrocytes, and osteocytes. They function to maintain the tissue matrix and keep the tissue healthy.
Fibers of the Connective Tissue: The extracellular matrix of connective tissue is composed of fibers and ground substance. The three types of fibers found in connective tissue are: collagen fibers, reticular fibers, and elastic fibers. Collagen Fibers resist tension (pulling forces) and contribute strength to connective tissue. Reticular Fibers- are bundles of a special type of collagen fibril. These short fibers cluster into a mesh like network that covers and supports the structures bordering the connective tissue. Elastic Fibers- contain the rubberlike protein elastin, which allows them to function like rubber bands. Elastic fibers recoil.
Ground Substance: The molecules that compose the ground substance are produced and secreted by the primary cell type of the connective tissue (fibroblasts, chondroblasts, or osteoblasts). The ground substance in most connective tissues is a gel-like material that consists of large sugar and sugar-protein molecules (proteoglycans and glycosaminoglycans). The fluid-filled ground substance functions to cushion and protect body structures, to withstand compressive stresses, or to hold the tissue fluid that bathes all the cells in our body.
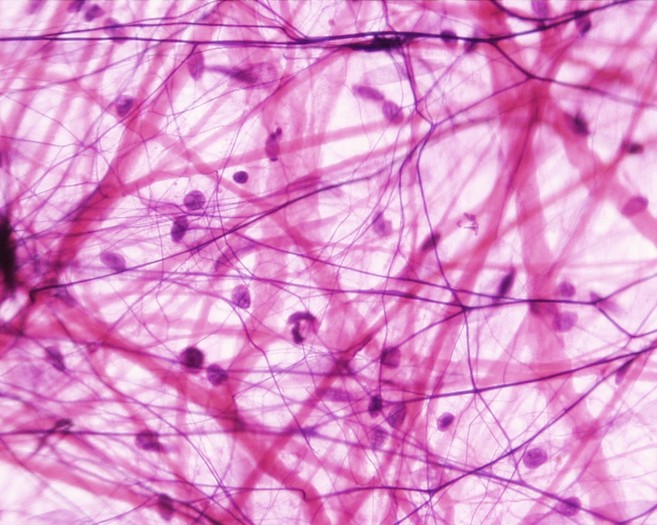
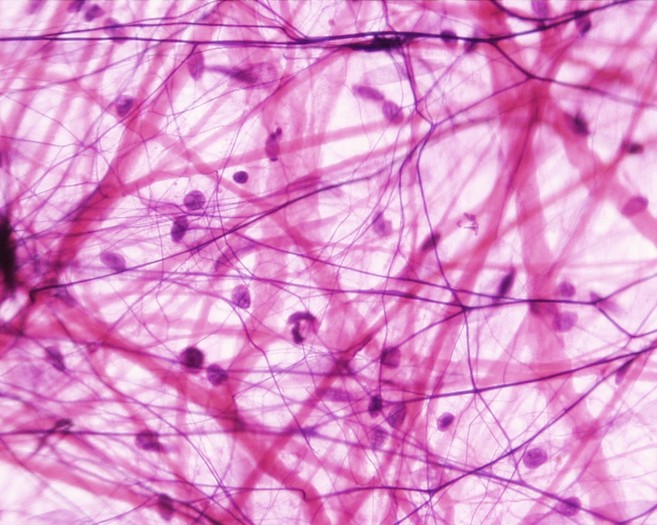 Areolar Loose Connective TIssue Proper Areolar Loose Connective TIssue Proper
Areolar Loose Connective Tissue Proper
Function: Loose packing, support, and nourishment for the structures with which it is associated
Location: Widely distributed throughout the body; substance on which epithelial basement membranes rest; packing between glands, muscles, and nerves; attaches the skin to underlying tissues.
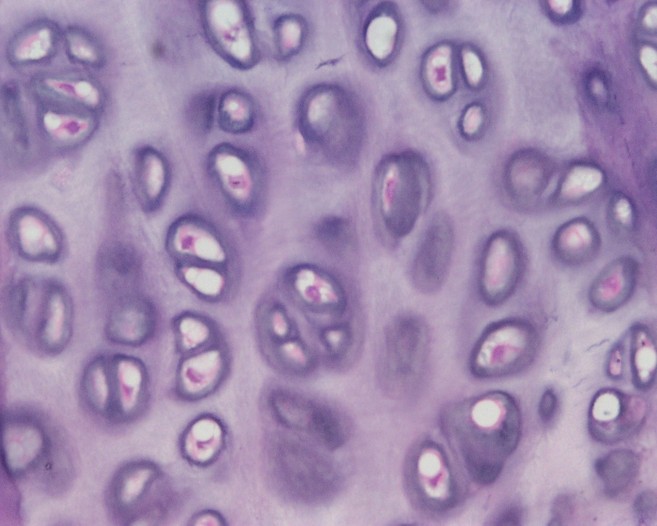
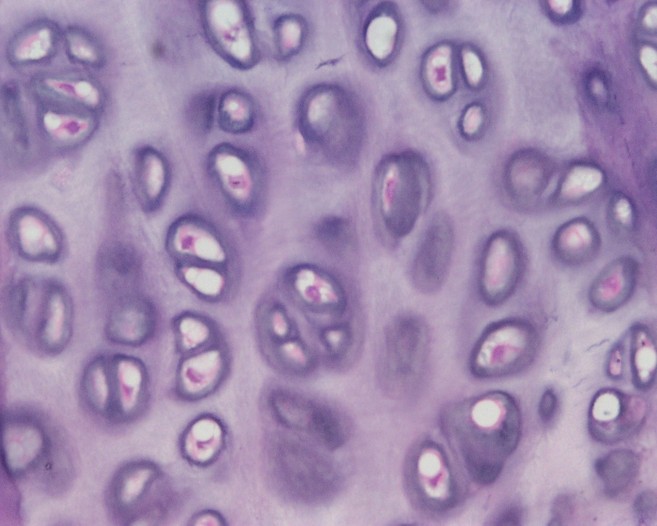 Elastic Cartilage Elastic Cartilage
Elastic Cartilage
Function: Provides rigidity with even more flexibility than hyaline cartilage because elastic fibers return to their original shape after being stretched.
Location: External ears, epiglottis, auditory tubes
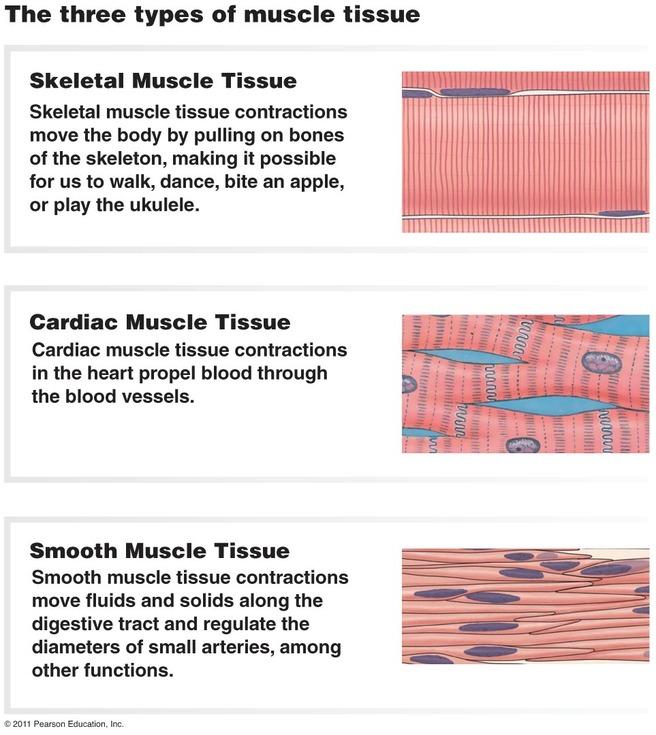
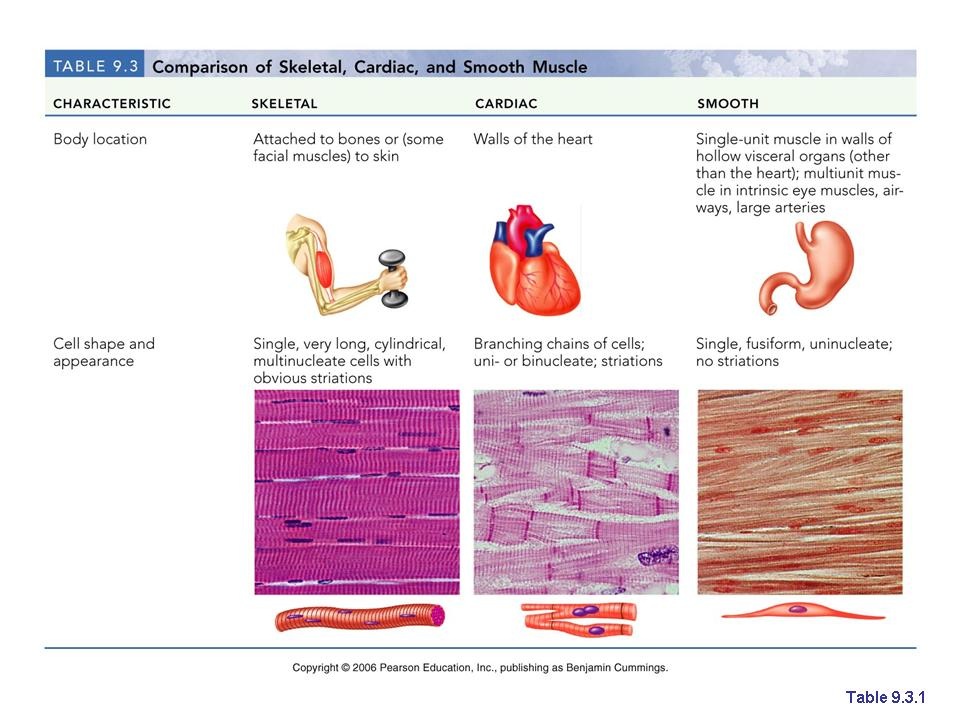 Muscle Tissues Muscle Tissue- The main characteristic of muscle tissue is its ability to contract or shorten, making movement possible. Muscle contraction results from contractile proteins located within the muscle cells. Muscle cells are also called muscle fibers. The three types of muscle tissue are: skeletal, cardiac, and smooth.
Skeletal muscle is what we normally think of as "muscle". Skeletal muscle attaches to the skeleton and enables the body to move. Skeletal muscle is described as voluntary because a person can purposefully cause skeletal muscle contraction to achieve specific body movements.
Cardiac muscle is the muscle of the heart. It is responsible for pumping blood. Cardiac muscle is under involuntary control, although a person can learn to influence the heart rate by using techniques such as meditation and biofeedback. Cardiac muscles are cylindrical but much shorter than skeletal muscle cells. Cardiac muscles are striated and usually have one nucleus per cell. They are often branched and connected to one another by intercalated discs. The intercalated discs, which contain specialized gap junctions, are important in coordinating the contractions of cardiac muscle cells.
Smooth muscle forms the walls of hollow organs (except the heart); it is also found in the skin and the eyes. Smooth muscle is responsible for a number of functions, such as moving food through the digestive tract and emptying the urinary bladder. Like cardiac muscle, smooth muscle is controlled involuntarily. Smooth muscle cells are tapered at each end, having a single nucleus, and are not striated.
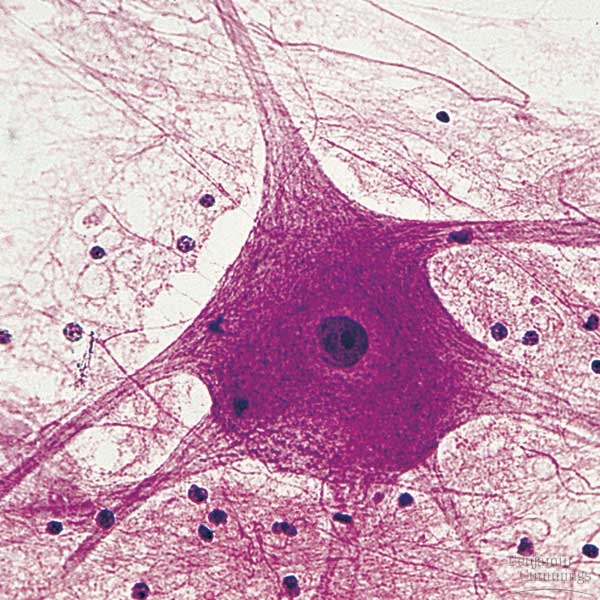 Nervous Tissue Nervous Tissue- forms the brain, spinal cord, and nerves. It is responsible for coordinating and controlling many body activities. Nervous tissue consists of neurons and support cells. The neuron, or nerve cell, is responsible for conducting action potentials. It is composed of three parts: a cell body, dendrites, and an axon. The cell body contains the nucleus and is the site of general cell functions. Dendrites and axons are nerve cell processes. Dendrites usually receive stimuli leading to electrical changes that either increase or decrease action potentials in the neuron's axon. Action potentials usually originate at the base of an axon where it joins the cell body and travel to the end of the axon. Neuroglia are the support cells of the nervous system; they nourish, protect, and insulate the neurons.
Function: Neurons transmit information in the form of action potentials, store information and integrate and evaluate data; neuroglia support, protect, and form specialized sheaths around axons.
Location: In the brain, spinal cord, and ganglia
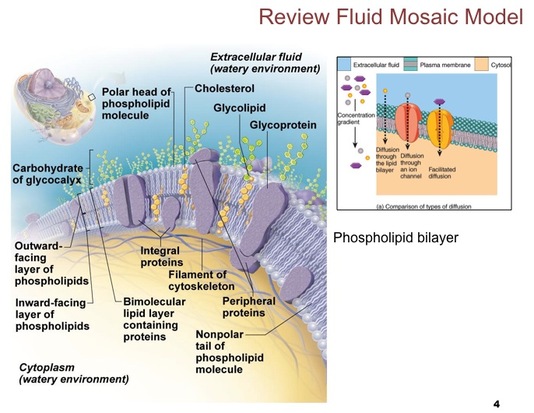
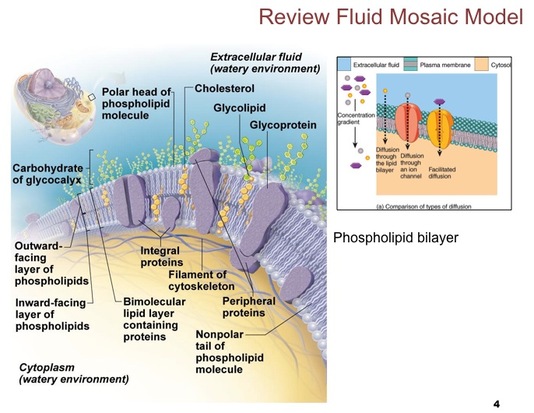 The membrane is composed of a bilayer of phospholipids and cholesterol with proteins "floating" in the membrane. The nonpolar hydrophobic region of each phospholipid molecule is directed toward the center of the membrane, and the polar hydrophilic region is directed toward the fluid environment either outside or inside the cell.
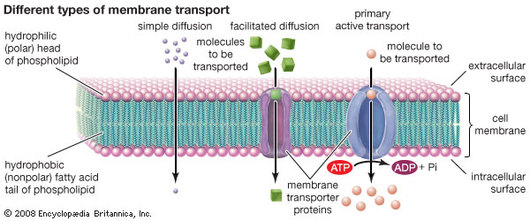
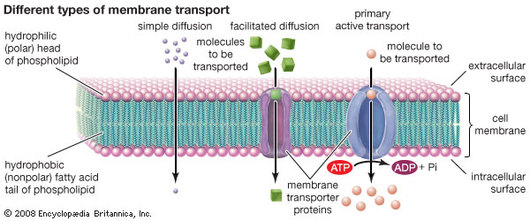 Simple Diffusion- Small, uncharged molecules, such as oxygen, carbon dioxide, and fat-soluble molecules, can pass freely through the lipid bilayer of the plasma membrane. Osmosis- The diffusion of water molecules across a membrane. Facilitated Diffusion- Water-soluble or charged molecules, such as glucose, amino acids, and ions, cannot pass through the lipid bilayer by simple diffusion. Such substances can cross the plasma membrane only by means of specific transport mechanisms that use integral proteins to carry or pump molecules across the membrane or to form channels through which specific molecules pass. Active Transport- The movement of molecules across the plasma membrane across their concentration gradient.
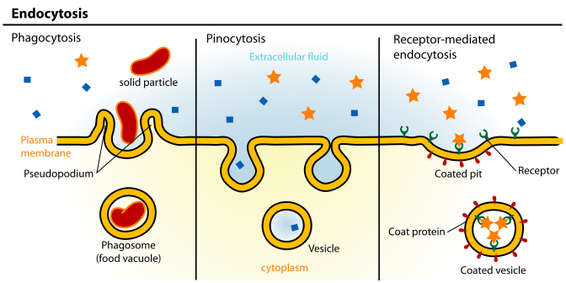
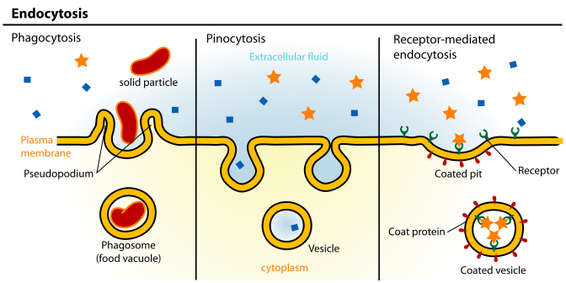 Phagocytosis- "Cell eating." The cell engulfs a large particle by forming pseudopods ("false feet") around it and enclosing it within a membrane sac called a phagosome. THe phagosome then combines with a lysosome, and its contents are digested. Vesicle may or may not be protein-coated but has receptors capable of binding to microorganisms or solid particles. Pinocytosis- The cell "gulps" drops of extracellular fluid containing solutes into tiny vesicles. No receptors are used, so the process is nonspecific. Most vesicles are protein-coated. Receptor-Mediated Endocytosis- Extracellular substances bind to specific receptor protein-coated pits, enabling the cell to ingest and concentrate specific substances in protein-coated vesicles. The ingested substance may simply be released inside the cell, or combined with a lysosome to digest contents. Receptors are recycled to the plasma membrane in vesicles.
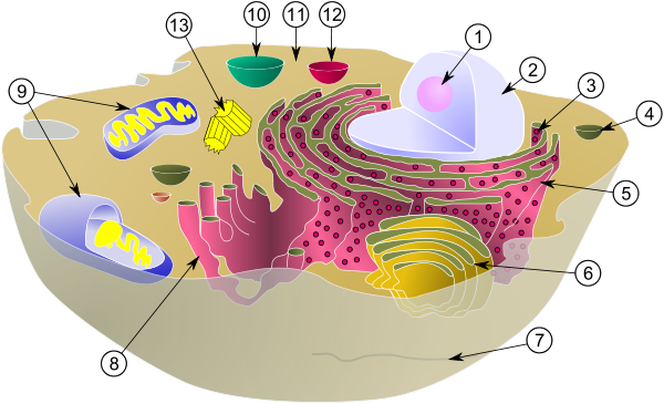
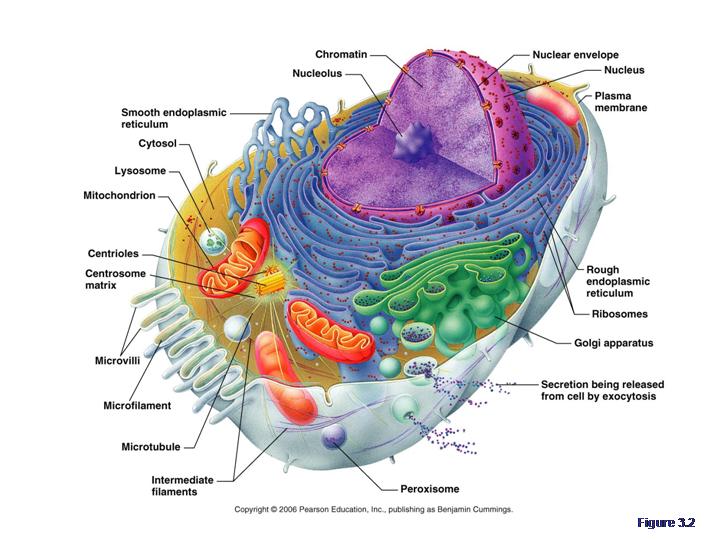
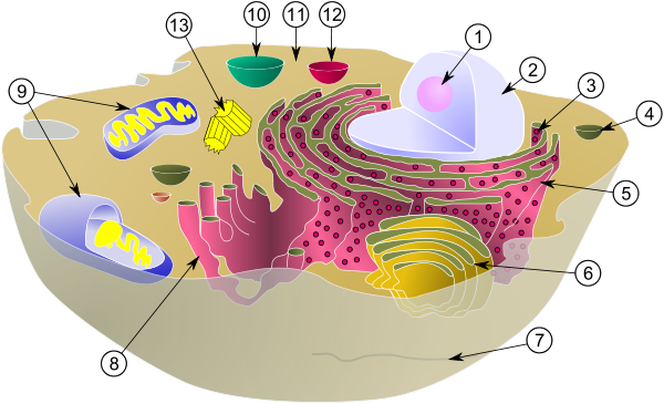
Match the Organelle with its function!
A. Site of Protein Synthesis
B. Makes proteins that are secreted from the cell; makes the cell's membranes
C. Site of lipid synthesis, lipid metabolism, and drug detoxification
D. Packages, modifies, and segregates proteins for secretion from the cell, inclusion in lysosomes, and incorporation into the plasma membrane
E. Sites of intracellular indigestion
F. Sites of intracellular digestion
G. Site of ATP synthesis; powerhouse of the cell
H. The enzymes detoxify a number of toxic substances; the most important enzyme, catalase, breaks down hydrogen peroxide
I. Involved in muscle contraction and other types of intracellular movement; help form the cell's cytoskeleton
J. Involved in muscle contraction and other types of intracellular movement; helps form the cell's cytoskeleton
K. The stable cytoskeleton elements; resist tension forces acting on the cell
L. Support the cell and give it shape; involved in intracellular and cellular movements; form centrioles
M. Organize a microtubule network during mitosis to form the spindle and asters; form the bases of cilia and flagella
N. Control center of the cell; responsible for transmitting genetic information and providing the instructions for protein synthesis
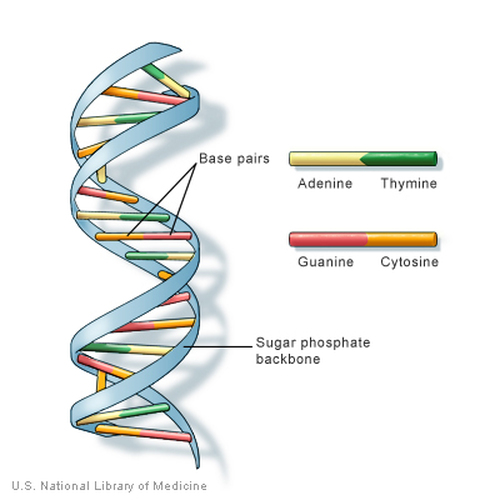
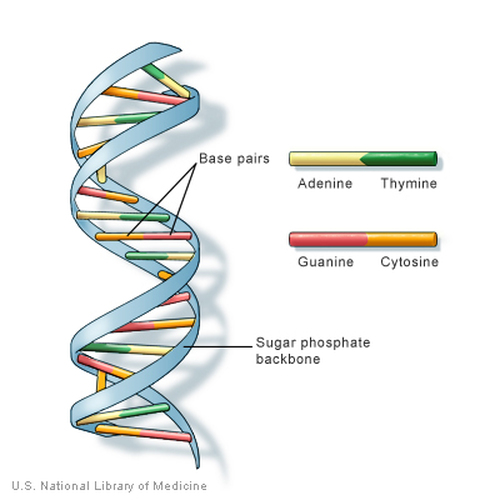 The DNA is a long double helix that resembles a spiral staircase. THis double helix is in turn composed of four kinds of subunits called nucleotides, each of which contains a distinct base. These bases- thymine, adenine, cytosine, and guanine- bind to form the "stairs" of the "staircase" and to hold the DNA helix together. The double helix of DNA is packed with protein molecules and coiled ins trends of increasing structural complexity and thickness. The DNA molecule plus the proteins form chromatin. Each two turns of the DNA helix is packed with eight disc-shaped protein molecules called histones. Each cluster of DNA and histones is called a nucleosome. In an electron micrograph of chromatin, the nucleosomes have the appearance of beads on a string. Chromatin in this form is called extended chromatin. Further coiling of the nucleosomes forms a tight helical fiber. THese thick fibers of chromatin are called condensed chromatin.
 An element is the simplest type of matter having unique chemical properties. About 96% of the body's weight results from the elements oxygen, carbon, hydrogen, and nitrogen. Many other elements are found in the body which play important roles. Calcium, for example, helps form bones, and sodium ions are essential for neuronal activity. Some of the other elements are present in very small amounts but are still essential for life.
|



 RSS Feed
RSS Feed