The Integumentary System consists of the hair, nails, and skin. Integument means covering, and the integumentary system covers the outside of the body.
Functions of the Integumentary System: Protection, Sensation, Vitamin D production, Temperature Regulation, and Excretion.
Functions of the Integumentary System: Protection, Sensation, Vitamin D production, Temperature Regulation, and Excretion.
The Skin is made up of two major tissue layers. The Epidermis is the most superficial layer of the skin. It is a layer of epithelial tissue that rests on the dermis, a layer of dense connective tissue. The epidermis prevents water loss and resists abrasion. The dermis is responsible for most of the skin's structural strength. The skin rests on the subcutaneous tissue, which is a layer of connective tissue. The subcutaneous tissue is not part of the skin, but it does connect the skin to underlying muscle or bone.
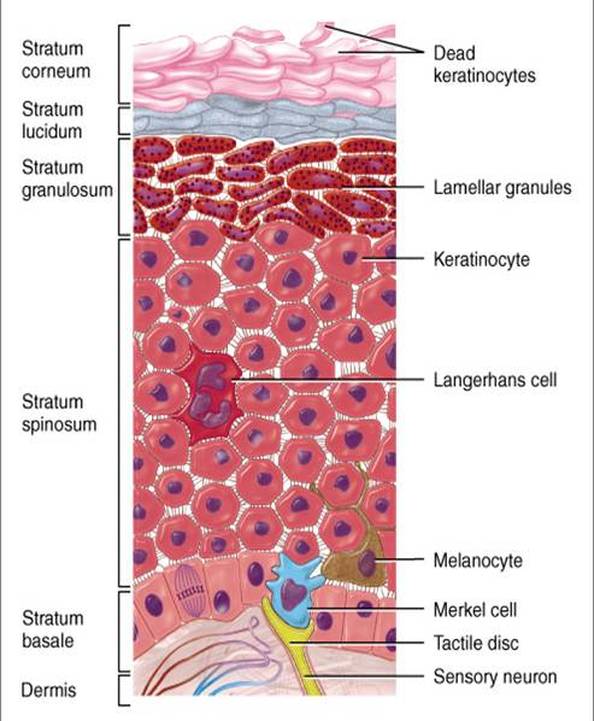
The Epidermis is a keratinized stratified squamous epithelium that contains four distinct types of cells: keratinocytes, melanocytes, tactile epithelial cells, and dendritic cells. Keratinocytes, the most abundant epidermal cell, produce keratin, a tough fibrous protein that gives the epidermis its protective properties. Keratinocytes also produce produce antibiotics and enzymes that detoxify the harmful chemicals to which our skin is exposed. Keratinocytes arise in the deepest part of the epidermis from cells that undergo almost continuous mitosis. As these cells are pushed up by the production of new cells beneath them, they make the keratin that eventually fills their cytoplasm. By the time they approach the skin surface, they are dead, flat sacs completely filled with keratin.
Layers of the Epidermis:
Stratum Basale- deepest epidermal layer, firmly attached to the underlying dermis along a wavy borderline. It consists of a single row of cells, mostly stem cells representing the youngest keratinocytes. These cells divide rapidly, and many mitotic nuclei are visible. Tactile epithelial cells or merkel cells are distributed sparsely among the keratinocytes. Each tactile epithelial cell is intimately associated with a dislike sensory nerve ending and functions as a receptor for touch. About 10%-25% of the cells in the stratum basal are melanocytes, which make the dark skin pigment melanin.
Stratum Spinosum- is several layers thick. Cells of the stratum spinosum consist of a tension-resisting protein pre-keratin. Scattered among the keratinocytes of the stratum spinosum are dendritic cells. Dendritic cells police the outer body surface, using receptor-mediated endocytosis to take up foreign proteins (antigens) that have invaded the epidermis.
Stratum Granulosum- consists of one to five layers of flattened keratinocytes. Along with abundant pre-keratin intermediate filaments, these cells also contain keratohyalin granules and lamellated granules. The keratohyalin granules help form keratin in the more superficial layers. The lamellated granules contain a waterproofing glycolipid that is secreted into the extracellular space and plays a major role in slowing water loss across the epidermis. Furthermore, the plasma membranes of the cells thicken so that they become more resistant to destruction.
Stratum Lucidum- occurs in thick skin. Consists of a few rows of flat, dead keratinocytes.
Stratum Corneum- The most external part of the epidermis, consists of many layers of cells. Its dead keratinocytes are flat sacs completely filled with keratin because their nuclei and organelles disintegrated upon cell death. Keratin consists of the pre-keratin intermediate filament embedded in a "glue" from the keratohyalin granules. Both the keratin and the thickened plasma membranes of cells in the stratum corneum protect the skin against abrasion and penetration. Additionally, the glycolipid between its cells keep this later waterproof.
The Dermis, is a strong, flexible connective tissue. The cells of the dermis are typical of any connective tissue proper: fibroblasts, macrophages, mast cells, and scattered white blood cells. The fibers are: collagen, elastic, and reticular.
The Dermis is richly supplied with nerve fibers and blood vessels. The dermal blood vessels consist of two vascular plexuses (a plexus is a network of converging and diverging vessels). The deep dermal plexus is located between the hypodermic and the dermis. It nourishes the hypodermic and the structures located within the deeper portions of the dermis. The more superficial sub papillary plexus, located just below the dermal papillae, supplies the more superficial dermal structures, the dermal papillae, and the epidermis. Dermal blood vessels do more than just nourish the dermis and overlying epidermis; they also perform a critical role in temperature regulation.
The dermis has two layers: papillary and reticular. The papillary layer, the superficial 20% of the dermis, is areolar connective tissue containing very thin collagen and elastic fibers. It includes the dermal papillae, finger-like projections that extend into the overlying epidermis. These projections of the dermal papillae into the epidermis increase the surface area for exchange of gases, nutrients, and waste products between these laters. The deeper reticular layer, which accounts for about 80% of the thickness of the dermis, is dense irregular connective tissue. Its extracellular matrix contains thick bundles of interlacing collagen and elastic fibers that run in many different planes. The reticular layer is named for its networks of collagen fibers; the name does not imply any special abundance of reticular fibers. Separations or less dense regions between the collagen bundles form the cleavage lines or tension lines of the skin.
The Dermis is richly supplied with nerve fibers and blood vessels. The dermal blood vessels consist of two vascular plexuses (a plexus is a network of converging and diverging vessels). The deep dermal plexus is located between the hypodermic and the dermis. It nourishes the hypodermic and the structures located within the deeper portions of the dermis. The more superficial sub papillary plexus, located just below the dermal papillae, supplies the more superficial dermal structures, the dermal papillae, and the epidermis. Dermal blood vessels do more than just nourish the dermis and overlying epidermis; they also perform a critical role in temperature regulation.
The dermis has two layers: papillary and reticular. The papillary layer, the superficial 20% of the dermis, is areolar connective tissue containing very thin collagen and elastic fibers. It includes the dermal papillae, finger-like projections that extend into the overlying epidermis. These projections of the dermal papillae into the epidermis increase the surface area for exchange of gases, nutrients, and waste products between these laters. The deeper reticular layer, which accounts for about 80% of the thickness of the dermis, is dense irregular connective tissue. Its extracellular matrix contains thick bundles of interlacing collagen and elastic fibers that run in many different planes. The reticular layer is named for its networks of collagen fibers; the name does not imply any special abundance of reticular fibers. Separations or less dense regions between the collagen bundles form the cleavage lines or tension lines of the skin.
The Hypodermis also called the superficial fascia and subcutaneous layer consists of both areolar and adipose connective tissue, but adipose tissue normally predominates. Besides storing fat, the hypodermic anchors the skin to the underlined structures, but loosely enough that the skin can slide relatively freely over those structures.
Nails are made of dead, keratinized cells. The hard keratin that predominates in hairs and nails differs from the soft keratin that is found in typical epidermal cells. Each nail has a distal free edge, a body (the visible attached part) and a root (the proximal part embedded in the skin). The nail rests on a bed of epidermis called the nail bed.
Hair is a flexible strand made of dead cells filled with card keratin. The chief parts of hair are the root, the part embedded in the skin, and the shaft, the part that projects above the skin surface. A hair consists of three concentric laters of keratinized cells. Its central core, the medulla, consists of large cells and air spaces. The medulla is absent in fine hairs. The cortex, surrounding the medulla, consists of several layers of flattened cells. The outermost cuticle is a single later of cells that overlap one another from below like shingles on a roof. This shingle pattern helps to keep neighboring hairs apart so that the hair does not mat.
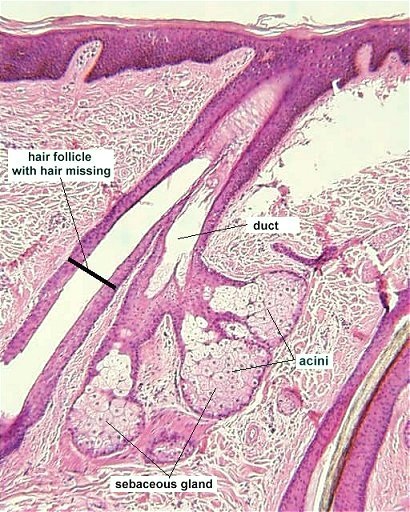
Sebaceous Glands are the skin's oil glands. They are simple alveolar glands with several alveoli opening into a single duct, but the alveoli are actually filled with cells, so there is no lumen (central cavity). THeir oily product is called sebum.
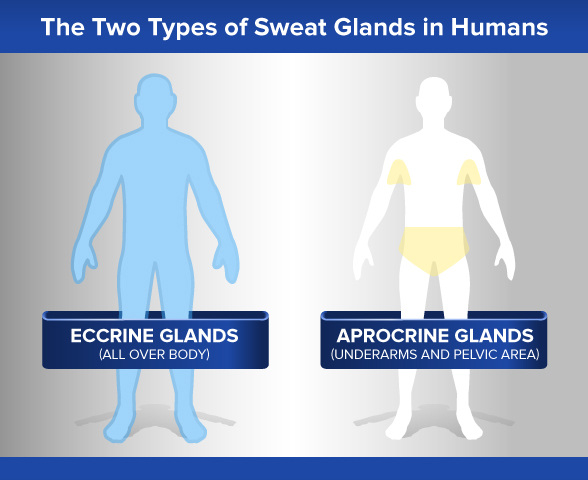
There are two types of sweat glands: Eccrine glands and Apocrine glands.
Eccrine glands are by far the more numerous type and produce true sweat. They are most abundant on the palms, soles, and forehead. Each is a coiled version of a simple tubular gland. The coiled, secretory base lies in the deep dermis and hypodermic, and the fact runs superficially to open at the skin surface through a funnel shaped pore.
Apocrine glands are mostly confined to the axillary, anal, and genital areas. They are larger than eccrine glands and produce a special kind of sweat consisting of fatty substances and proteins, in addition to the components of true sweat. For this reason, apocrine sweat is viscous and sometimes has a milky or yellow color. THis product is odorless when first secreted, but its organic molecules are decomposed by bacteria on the skin, it takes on a musky smell. This is the source of body odor.
Eccrine glands are by far the more numerous type and produce true sweat. They are most abundant on the palms, soles, and forehead. Each is a coiled version of a simple tubular gland. The coiled, secretory base lies in the deep dermis and hypodermic, and the fact runs superficially to open at the skin surface through a funnel shaped pore.
Apocrine glands are mostly confined to the axillary, anal, and genital areas. They are larger than eccrine glands and produce a special kind of sweat consisting of fatty substances and proteins, in addition to the components of true sweat. For this reason, apocrine sweat is viscous and sometimes has a milky or yellow color. THis product is odorless when first secreted, but its organic molecules are decomposed by bacteria on the skin, it takes on a musky smell. This is the source of body odor.
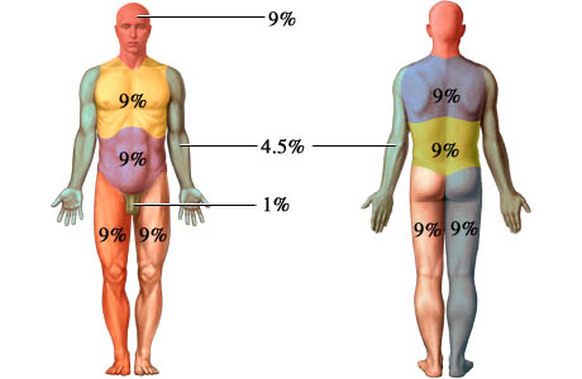
Burns are classified by their severity as first-, second-, or third-degree burns.
First-degree burns- Only the epidermis is damaged. Symptoms include redness, swelling, and pain: the typical inflammatory reaction to tissue damage. Generally first-degree burns heal in a few days without special attention.
Second-degree burns- involve injury to the epidermis and the upper part of the dermis. Symptoms resemble those of first-degree burns, but blisters also appear as fluid accumulates between the epidermal and dermal layers. The skin regenerates with little or no scarring in 3 to 4 weeks if care is taken to prevent infection. First-and second-degree burns are considered partial-thickness burns.
Third-Degree burns- consume the entire thickness of the skin, and thus are full-thickness burns. The burned area appears white, red, or blackened. Although the skin might eventually regenerate, it is usually impossible to wait for this because of fluid loss and infection. Therefore skin from other parts of the patient's body must be grafted onto the burned area.
First-degree burns- Only the epidermis is damaged. Symptoms include redness, swelling, and pain: the typical inflammatory reaction to tissue damage. Generally first-degree burns heal in a few days without special attention.
Second-degree burns- involve injury to the epidermis and the upper part of the dermis. Symptoms resemble those of first-degree burns, but blisters also appear as fluid accumulates between the epidermal and dermal layers. The skin regenerates with little or no scarring in 3 to 4 weeks if care is taken to prevent infection. First-and second-degree burns are considered partial-thickness burns.
Third-Degree burns- consume the entire thickness of the skin, and thus are full-thickness burns. The burned area appears white, red, or blackened. Although the skin might eventually regenerate, it is usually impossible to wait for this because of fluid loss and infection. Therefore skin from other parts of the patient's body must be grafted onto the burned area.
Skin cancer is the most common type of cancer, with about a million new cases appearing each year in the United States.
Melanoma- a cancer of melanocytes, is the most dangerous type of skin cancer. Melanocytes are derived from neural crest cells, which wander widely during embryonic development. This predisposition for migration may explain the invasive nature of melanoma. Melanoma accounts for only about 1 out of every 20 skin cancers, but it is increasing rapidly in countries with light-skinned populations- by 3% to 8% per year in the United States. Melanoma can originate wherever there is pigment, but it often arises from existing moles, usually appearing as an expanded dark patch. Because melanoma cells metastasis rapidly into surrounding circulatory vessels, the key to surviving melanoma is early detection. Most people do not survie this cancer if the lesion has grown over 4mm thick. Melanoma is resistant to chemotherapy and current immunotherapy treatment, although vaccines are being tested.
Melanoma- a cancer of melanocytes, is the most dangerous type of skin cancer. Melanocytes are derived from neural crest cells, which wander widely during embryonic development. This predisposition for migration may explain the invasive nature of melanoma. Melanoma accounts for only about 1 out of every 20 skin cancers, but it is increasing rapidly in countries with light-skinned populations- by 3% to 8% per year in the United States. Melanoma can originate wherever there is pigment, but it often arises from existing moles, usually appearing as an expanded dark patch. Because melanoma cells metastasis rapidly into surrounding circulatory vessels, the key to surviving melanoma is early detection. Most people do not survie this cancer if the lesion has grown over 4mm thick. Melanoma is resistant to chemotherapy and current immunotherapy treatment, although vaccines are being tested.

 RSS Feed
RSS Feed