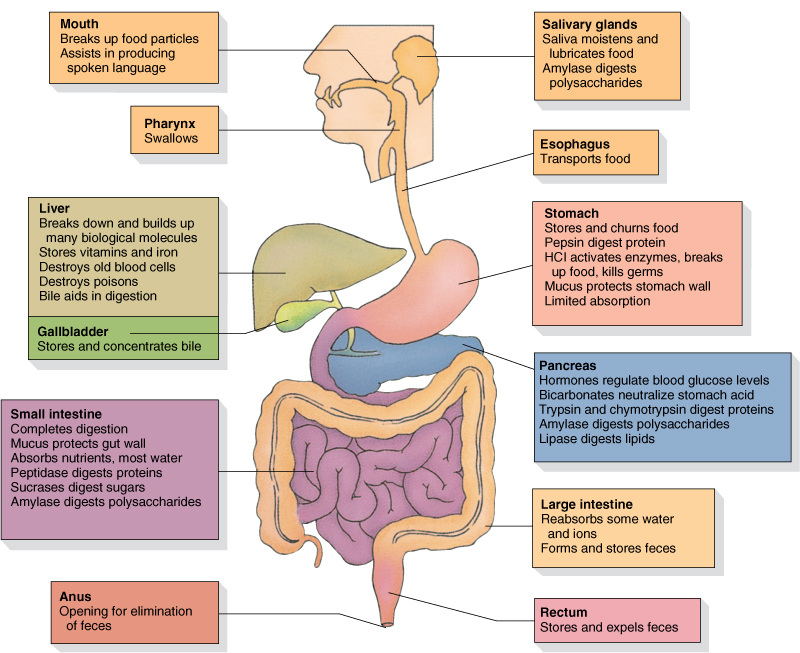
Functions of the Digestive System:
- Ingestion of food
- Digestion of food
- Absorption of nutrients
- Elimination of wastes
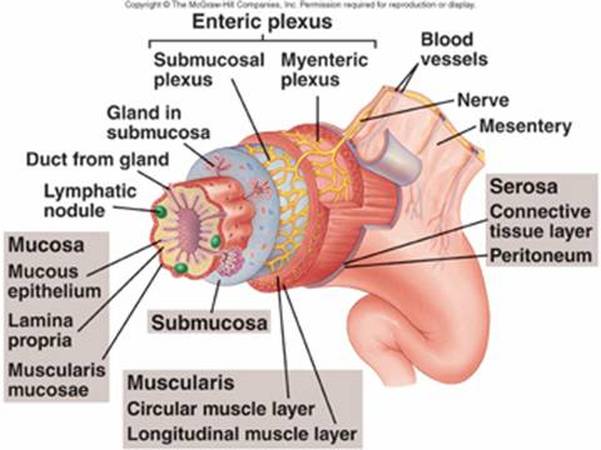
Histology of the Digestive System:
- The innermost tunic, the mucosa, consists of mucous epithelium, a loose connective tissue called the lamina propria, and a thin smooth muscle layer, the muscularis mucosae.
- The submucosa lies just outside the mucosa. It is a thick layer of loose connective tissue containing nerves, blood vessels, and small glands. An extensive network of nerve cell processes forms a plexus (network). Autonomic nerves innervate this plexus.
- The next tunic is the muscularis. In most parts of the digestive tract it consists of an inner layer of circular smooth muscle and an outer layer of longitudinal smooth muscle. Another nerve plexus, also innervated by autonomic nerves, lies between the two muscle layers. Together, the nerve plexuses of the submucosa and muscular is compose the enteric nervous system.
- The fourth, or outermost, layer of the digestive tract is either a serosa or an adventitia. The serosa consists of the peritoneum, which is a smooth epithelial layer, and its underlying connective tissue. Regions of the digestive tract not covered by peritoneum are covered by a connective tissue layer called the adventitia, which is continuous with the surrounding connective tissue.
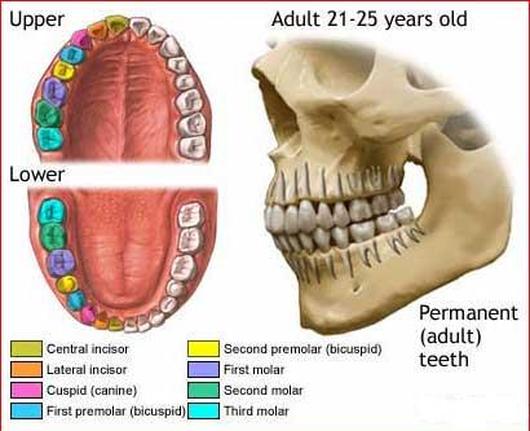
Teeth:
There are 32 teeth in the normal adult mouth, located in the mandible and maxillae. The teeth can be divided into quadrants: right upper, left upper, right lower, and left lower. In adults, each quadrant contains one central and one lateral incisor; first and second premolars; and first, second, and third molars. The thirst molars are called wisdom teeth.
The teeth of adults are called permanent teeth, or secondary teeth. Most of them are replacements for the 20 primary teeth, or deciduous teeth, also called milk or baby teeth, which are lost during childhood.
Each tooth consists of a crown with one or more cusps (points), a neck, and a root. The center of the tooth is a pump cavity, which is filled with blood vessels, nerves, and a connective tissue, called pulp. The pulp cavity is surrounded by a living, cellular, bonelike tissue called dentin. The dentin of the tooth crown is covered by an extremely hard, acellular substance called enamel, which protects the tooth against abrasion and acids produced by bacteria in the mouth. The surface of the dentin in the root is covered with cementum, which helps anchor the tooth in the jaw.
There are 32 teeth in the normal adult mouth, located in the mandible and maxillae. The teeth can be divided into quadrants: right upper, left upper, right lower, and left lower. In adults, each quadrant contains one central and one lateral incisor; first and second premolars; and first, second, and third molars. The thirst molars are called wisdom teeth.
The teeth of adults are called permanent teeth, or secondary teeth. Most of them are replacements for the 20 primary teeth, or deciduous teeth, also called milk or baby teeth, which are lost during childhood.
Each tooth consists of a crown with one or more cusps (points), a neck, and a root. The center of the tooth is a pump cavity, which is filled with blood vessels, nerves, and a connective tissue, called pulp. The pulp cavity is surrounded by a living, cellular, bonelike tissue called dentin. The dentin of the tooth crown is covered by an extremely hard, acellular substance called enamel, which protects the tooth against abrasion and acids produced by bacteria in the mouth. The surface of the dentin in the root is covered with cementum, which helps anchor the tooth in the jaw.
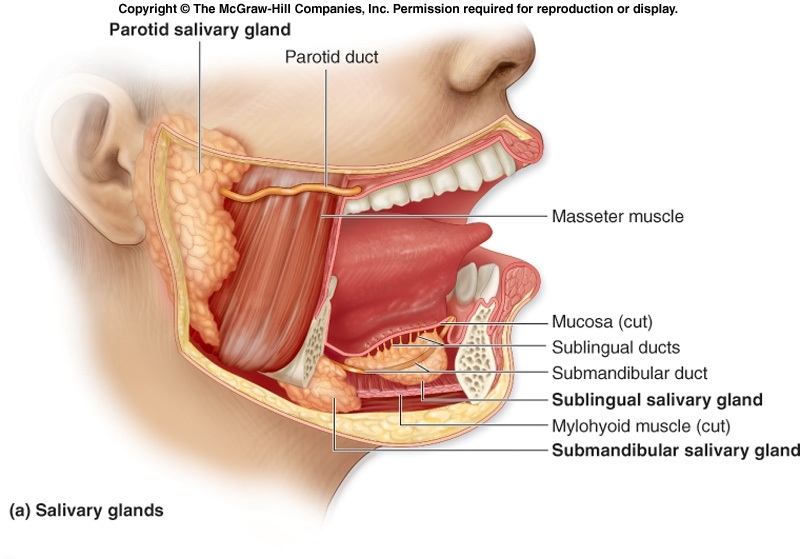
Salivary Glands:
- Parotid Gland- serous glands located just anterior to each ear. Parotid ducts enter the oral cavity adjacent to the second upper molars.
- Submandibular Glad- produce more serous than mucous secretions. Each gland can be felt as a soft lump along the inferior border of the mandible. The submandibular ducts open into the oral cavity on each side of the frenulum of the tongue.
- The sublingual glands- the smallest of the three paired salivary glands, produce primarily mucous secretions. They lie immediately below the mucous membrane in the floor of the oral cavity. Each sublingual gland has 10-12 small ducts opening onto the floor of the oral cavity.
Events During the Three Phases of Swallowing:
- During the voluntary phase, a bolus of food is pushed by the tongue against the hard and soft palates and posteriorly toward the oropharynx.
- During the pharyngeal phase, the soft palate is elevated, closing off the nasopharynx. The pharynx and larynx are elevated.
- Successive constriction of the pharyngeal constrictors from superior to inferior forces the bolus through the pharynx and into the esophagus. As this occurs, the vestibular and vocal folds expand medially to close the passage of the larynx. The epiglottis is bent down over the opening of the larynx largely by the force of the bolus pressing against it.
- As the inferior constrictor contracts, the upper esophageal sphincter relaxes, allowing the bolus to enter the esophagus.
- During the esophageal phase, the bolus is moved by peristaltic contractions of the esophagus toward the stomach
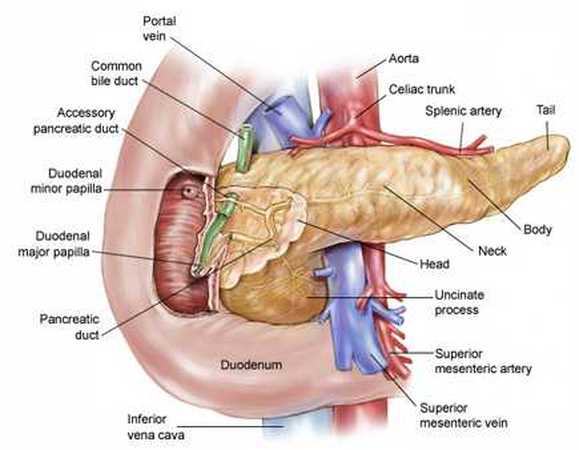
Flow of Bile and Pancreatic Secretions through the Duct system of the Liver, Gallbladder, & Pancreas:
- The hepatic ducts from the liver lobes combine to form the common hepatic duct.
- The common hepatic duct combines with the cystic duct from the gallbladder to form the common bile duct.
- The common bile duct joins the pancreatic duct.
- The combined duct empties into the duodenum at the duodenal papilla.
- Pancreatic secretions may also enter the duodenum through an accessory pancreatic duct, which also empties into the duodenum.
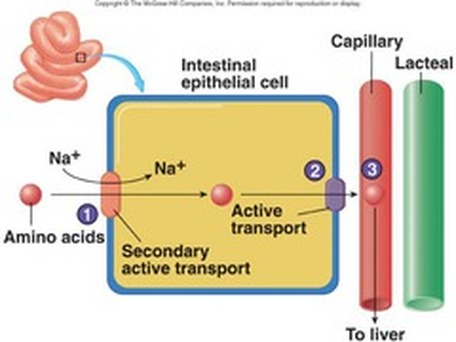
Lipid Transport:
- Bile salts surround fatty acids and monoglycerides to form micelles.
- Micelles attach to the cell membranes of intestinal epithelial cells, and the fatty acids and monoglycerides pass by simple diffusion into the intestinal epithelial cells.
- Within the intestinal epithelial cell, the fatty acids and monoglycerides are converted to triglycerides; proteins coat the triglycerides to form chylomicrons, which move out of the intestinal epithelial cells by exocytosis.
- The chylomicrons enter lacteals of the intestinal villi and are carried through the lymphatic system to the general circulation.

 RSS Feed
RSS Feed