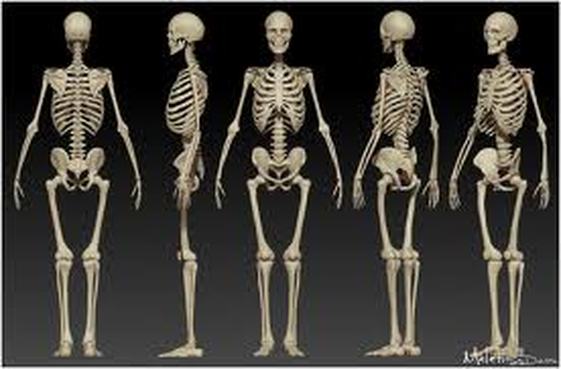
Functions of the Skeletal System:
1. Support
2. Protection
3. Movement
4.Storage
5. Blood cell production
1. Support
2. Protection
3. Movement
4.Storage
5. Blood cell production
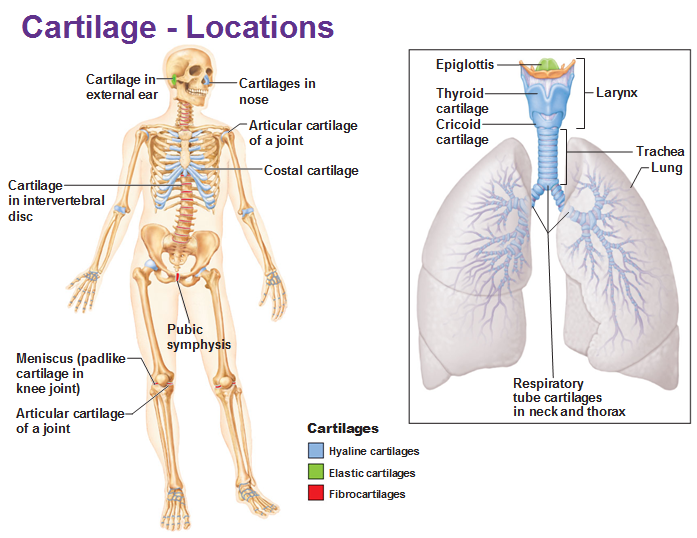
Types of Cartilage: Hyaline cartilage, elastic cartilage, and fibrocartilage.
Hyaline Cartilage: most abundant type of cartilage. The only type of fiber in the matrix is a collagen unit fibril, which forms networks that are too thin to be seen with alight microscope. The gelatinous ground substance holds large amounts of water; thus this tissue resists compression well. Hyaline cartilage proves support through flexibility and resilience.
Elastic Cartilage- its matrix contains many elastic fibers along with the delicate collagen fibrils. This cartilage is more elastic than hyaline and is better able to tolerate repeated bending.
Fibrocartilage- is an unusual tissue that resists both strong compression and strong tension (pulling) forces. It occurs in certain lima gents and certain cartilages that experience both of these forces.
Hyaline Cartilage: most abundant type of cartilage. The only type of fiber in the matrix is a collagen unit fibril, which forms networks that are too thin to be seen with alight microscope. The gelatinous ground substance holds large amounts of water; thus this tissue resists compression well. Hyaline cartilage proves support through flexibility and resilience.
Elastic Cartilage- its matrix contains many elastic fibers along with the delicate collagen fibrils. This cartilage is more elastic than hyaline and is better able to tolerate repeated bending.
Fibrocartilage- is an unusual tissue that resists both strong compression and strong tension (pulling) forces. It occurs in certain lima gents and certain cartilages that experience both of these forces.
Structure of aTypical Long Bone
The tubular diaphysis, or shaft, forms the long axis of a long bone. The epiphysis are the bone ends. The joint surface of each epiphysis is covered with a thin later of hyaline cartilage called the articular cartilage. Between the diaphysis and each epiphysis of an adult long bone is an epiphyseal line. This line is a remnant of the epiphyseal plate, a disc of hyaline cartilage that grows during childhood to lengthen the bone.
The Medullary Cavity- The interior of all bones consists largely of spongy bone. However, the very center of the diaphysis of a long bone contains no bone tissue at all and is called the medullary cavity or marrow cavity. This cavity is filled with yellow bone marrow.
Membranes:
Periosteum- covers the entire outer surface of each bone except on the ends of the epiphysis, where articular cartilage occurs.
Endosteum- covers the internal surfaces of bones. Specifically, endosteum covers the trabecular of spongy bone; it also lines the central canals of osteons.
The tubular diaphysis, or shaft, forms the long axis of a long bone. The epiphysis are the bone ends. The joint surface of each epiphysis is covered with a thin later of hyaline cartilage called the articular cartilage. Between the diaphysis and each epiphysis of an adult long bone is an epiphyseal line. This line is a remnant of the epiphyseal plate, a disc of hyaline cartilage that grows during childhood to lengthen the bone.
The Medullary Cavity- The interior of all bones consists largely of spongy bone. However, the very center of the diaphysis of a long bone contains no bone tissue at all and is called the medullary cavity or marrow cavity. This cavity is filled with yellow bone marrow.
Membranes:
Periosteum- covers the entire outer surface of each bone except on the ends of the epiphysis, where articular cartilage occurs.
Endosteum- covers the internal surfaces of bones. Specifically, endosteum covers the trabecular of spongy bone; it also lines the central canals of osteons.
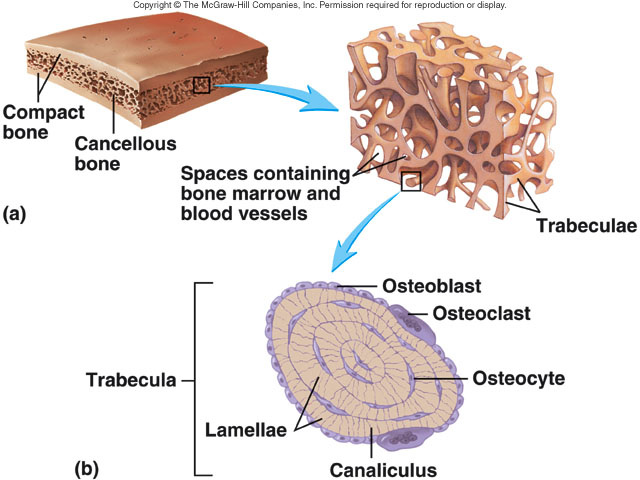
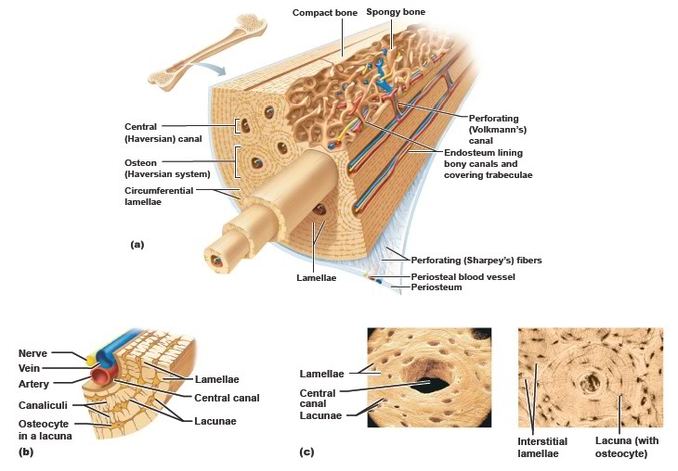
Almost every bone of the skeleton has a dense outer layer that looks smooth and solid to the naked eye. This eternal layer is compact bone. Internal to this is spongy bone also called trabecular bone, a honeycomb of small needle-like or flat pieces called trabeculae. In this network, the open spas between the trabecular are filled with red or yellow bone marrow.
Short, irregular, and flat bones have much the same composition as long bones: the periosteum-covered compact bone externally and endosteum-covered spongy bone internally. However, because these bones are not cylindrical, they have no diaphysis. They contain bone marrow (between the trabecular of their spongy bone), but no marrow cavity is present. In flat bones, the internal spongy bone is called diploe.
Short, irregular, and flat bones have much the same composition as long bones: the periosteum-covered compact bone externally and endosteum-covered spongy bone internally. However, because these bones are not cylindrical, they have no diaphysis. They contain bone marrow (between the trabecular of their spongy bone), but no marrow cavity is present. In flat bones, the internal spongy bone is called diploe.
An important structural component of compact bone is the osteon or Haversion System. Osteons are long, cylindrical structures oriented parallel to the long axis of the bone and to the main compression stresses. Functionally, osteons can be viewed as miniature weight-bearing pillars. Structurally, an osteon is a group of concentric tubes resembling the rings of tree trunk in cross section. Each of the tubes is a lamella, a layer of bone matrix in which the collagen fibers and mineral crystals align and run in a single direction.
Through the core of each osteon runs a canal called the central canal or Haversian canal. Like all internal bone cavities, it is lined by endosteum. The central canal contains its own blood vessels, which supply nutrients to the bone cells of the osteon, and its own nerve fibers.
Perforating canals also called Volkmann's canals, lie at right angles to the central canals and connect the blood and nerve supply of the periosteum to that of the central canals and the marrow cavity.
The mature bone cells, the osteocytes, are spider-shaped. Their bodies occupy small cavities in the solid matrix called lacunae, and their legs occupy thin tubes called canaliculi. These "little canals" run through the matrix, connecting neighboring lacunae to one another and to the nearest capillaries, such as those in the central canals.
Lying in between lamellae in compact bone are groups of incomplete lamellae called interstitial lamellae. These are simply the remains of old osteons that have been cut through by bone remodeling. Additionally, circumferential lamellae occur in the external and internal surfaces of the layer of compact bone; each of these lamellae extends around the entire circumference of the diaphysis. The circumferential lamellae effectively resist twisting of the entire long bone.
Through the core of each osteon runs a canal called the central canal or Haversian canal. Like all internal bone cavities, it is lined by endosteum. The central canal contains its own blood vessels, which supply nutrients to the bone cells of the osteon, and its own nerve fibers.
Perforating canals also called Volkmann's canals, lie at right angles to the central canals and connect the blood and nerve supply of the periosteum to that of the central canals and the marrow cavity.
The mature bone cells, the osteocytes, are spider-shaped. Their bodies occupy small cavities in the solid matrix called lacunae, and their legs occupy thin tubes called canaliculi. These "little canals" run through the matrix, connecting neighboring lacunae to one another and to the nearest capillaries, such as those in the central canals.
Lying in between lamellae in compact bone are groups of incomplete lamellae called interstitial lamellae. These are simply the remains of old osteons that have been cut through by bone remodeling. Additionally, circumferential lamellae occur in the external and internal surfaces of the layer of compact bone; each of these lamellae extends around the entire circumference of the diaphysis. The circumferential lamellae effectively resist twisting of the entire long bone.
Bone Development and Growth
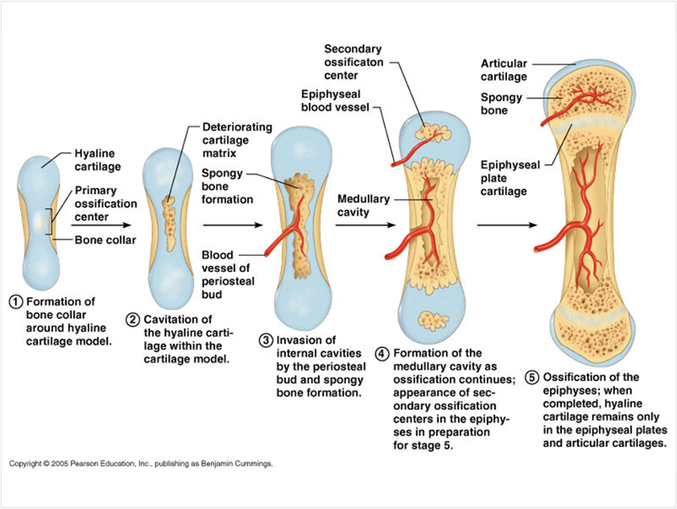
Osteogenesis and ossification are both names for the process of bone-tissue formation. Osteogenesis begins in the embryo, proceeds through childhood and adolescence as the skeleton grows, and then occurs at a slower rate in the adult as part of a continual remodeling of the full-grown skeleton.
Before week 8, the skeleton of the human embryo consists only of hyaline cartilage and some membranes of mesenchyme, and embryonic connective tissue. Bone tissue first appears in week 8 and eventually replaces most cartilage and mesenchymal membranes in the skeleton. Some bones, called membrane bones, develop from a mesenchymal membrane through a process called intramembranous ossification. Other bones develop as hyaline cartilage, which is replaced through a process called endochondral ossification. These bones are called endochondral bones or cartilage replacement bones.
Osteogenesis and ossification are both names for the process of bone-tissue formation. Osteogenesis begins in the embryo, proceeds through childhood and adolescence as the skeleton grows, and then occurs at a slower rate in the adult as part of a continual remodeling of the full-grown skeleton.
Before week 8, the skeleton of the human embryo consists only of hyaline cartilage and some membranes of mesenchyme, and embryonic connective tissue. Bone tissue first appears in week 8 and eventually replaces most cartilage and mesenchymal membranes in the skeleton. Some bones, called membrane bones, develop from a mesenchymal membrane through a process called intramembranous ossification. Other bones develop as hyaline cartilage, which is replaced through a process called endochondral ossification. These bones are called endochondral bones or cartilage replacement bones.
Repair of Bone Fractures
Despite their strength, bones are susceptible to fractures, or breaks. A fracture in which the bone breaks cleanly but does not penetrate the skin is a simple fracture. When broken ends of the bone protrude through the skin, the fracture is compound. A fracture is treated by reduction, realignment of the broken bone ends. In closed reduction, the bone ends are coaxed back into position by the physician's hands. In open reduction, the bone ends are joined surgically with pins or wires. After the broken bone is reduced, it is immobilized by a cast or traction to allow the healing process to begin. Healing time is about 6 to 8 weeks for a simple fracture, but it is longer for large, weight-bearing bones and for the bones of older people.
Despite their strength, bones are susceptible to fractures, or breaks. A fracture in which the bone breaks cleanly but does not penetrate the skin is a simple fracture. When broken ends of the bone protrude through the skin, the fracture is compound. A fracture is treated by reduction, realignment of the broken bone ends. In closed reduction, the bone ends are coaxed back into position by the physician's hands. In open reduction, the bone ends are joined surgically with pins or wires. After the broken bone is reduced, it is immobilized by a cast or traction to allow the healing process to begin. Healing time is about 6 to 8 weeks for a simple fracture, but it is longer for large, weight-bearing bones and for the bones of older people.
- Hematoma Formation. The fracture is usually accompanied by hemorrhaging. Blood vessels break in the periosteum and inside the bone, releasing blood that clots to form a hematoma.
- Fibrocartilaginous callus formation. WIthin a few days, new blood vessels grow into the clot. The periosteum and endosteum near the fracture site show a proliferation of bone-forming cells, which then invade the clot, filling it with repair tissue called soft callus. As fibers are produced, the soft callus becomes a dense connective tissue containing fibrocartilage and hyaline cartilage.
- Bony callus formation. within a week, the trabecular of new bone begins to form in the callus, mostly by endochondral ossification. These trabecular span the width of the callus and unite the two fragments of the broken bone. The callus is not called a bony callus or hard callus and its trabeculae grow thicker and stronger and become firm about 2 months after the injury.
- Bone remodeling. Over a period of many months, the bony callus is remodeled. The excess body material is removed from both the exterior of the bone shaft and the interior of the medullary cavity. Compact bone is laid down to reconstruct the shaft walls. The repaired area resembles the original unbroken bone region, because it responds to the same set of mechanical stresses.
 RSS Feed
RSS Feed