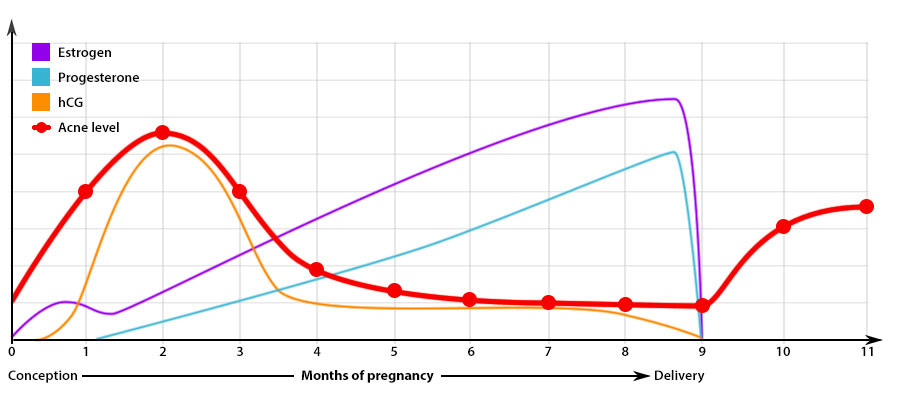
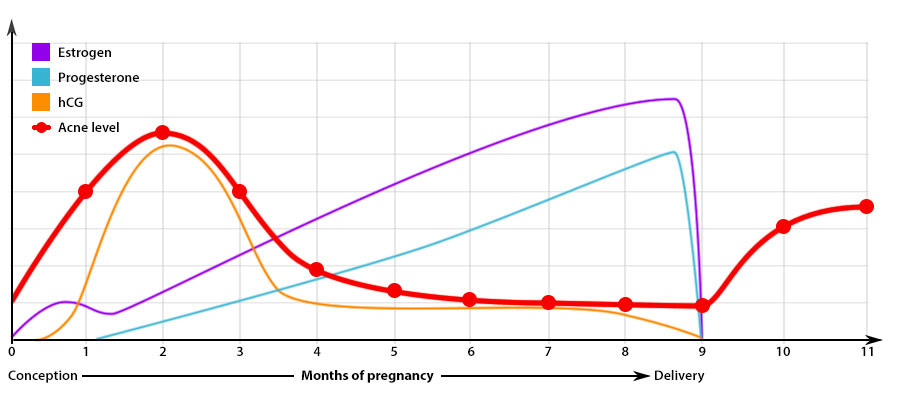
Hormone changes during Pregnancy
- First Trimester- Human chorionic gonadotropin (hCG) increases until it reaches a maximum concentration near the end of the first 3 months of pregnancy and then decreases to a low level thereafter.
- Second Trimester- Progesterone continues to increase until it levels off near the end of pregnancy. Early in pregnancy, progesterone is produced by the corpus luteum in the ovary; by the second trimester, production shifts to the placenta.
- Third Trimester- Estrogen increases slowly throughout pregnancy but increases more rapidly as the end of pregnancy approaches. Early in pregnancy, estrogen is produced only in the ovary; by the second trimester, production shifts to the placenta.
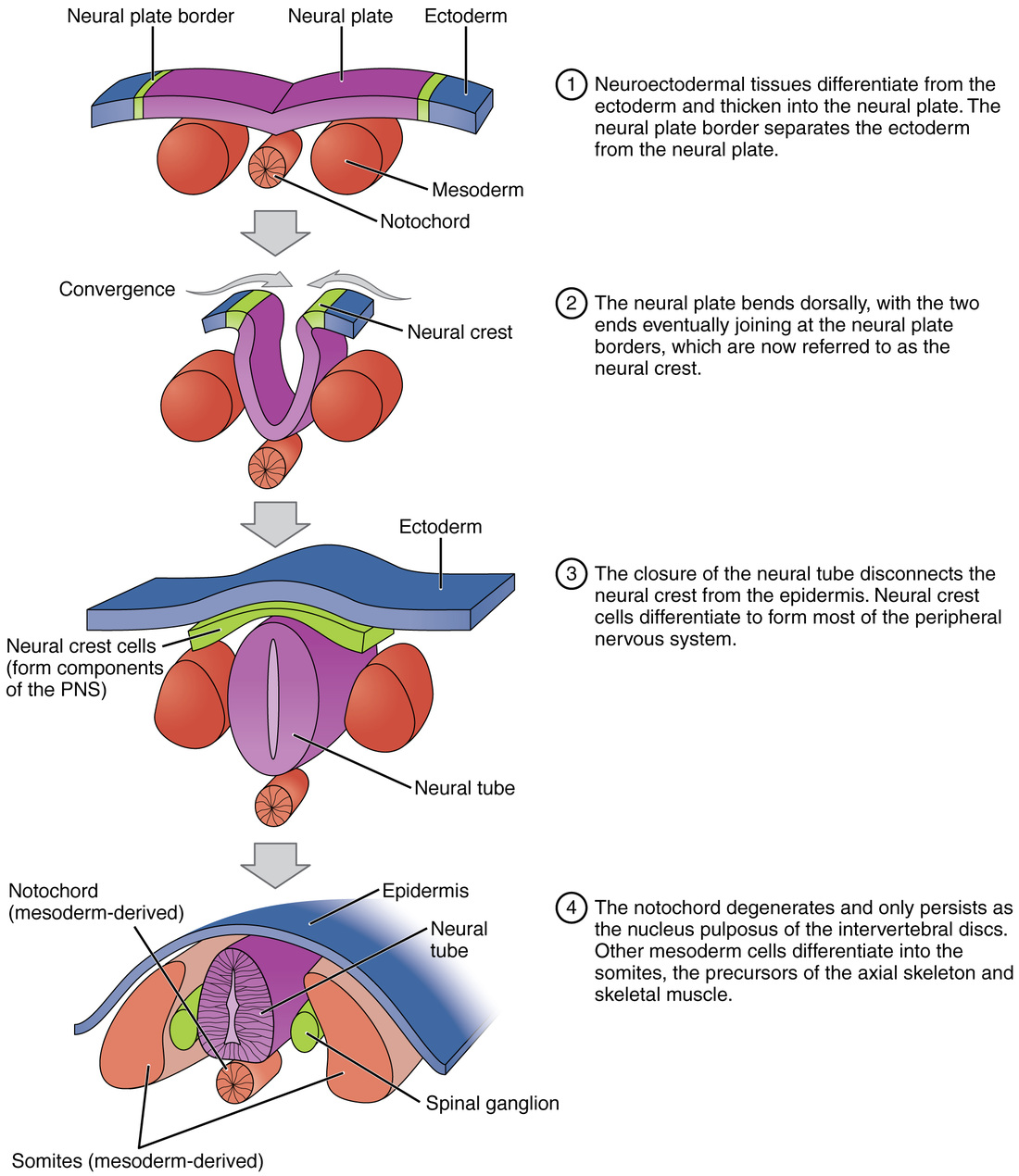
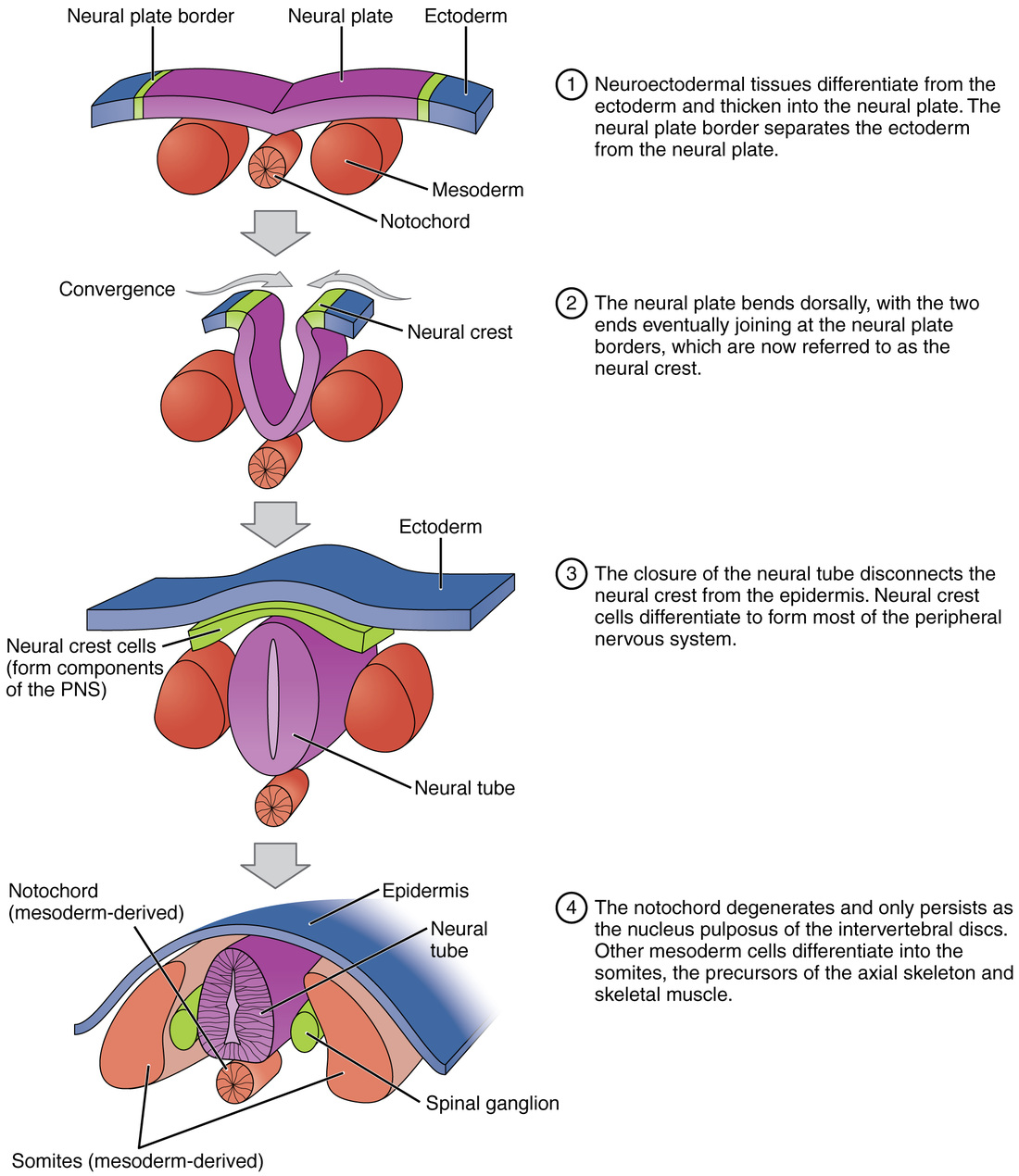
Formation of Neural Tube
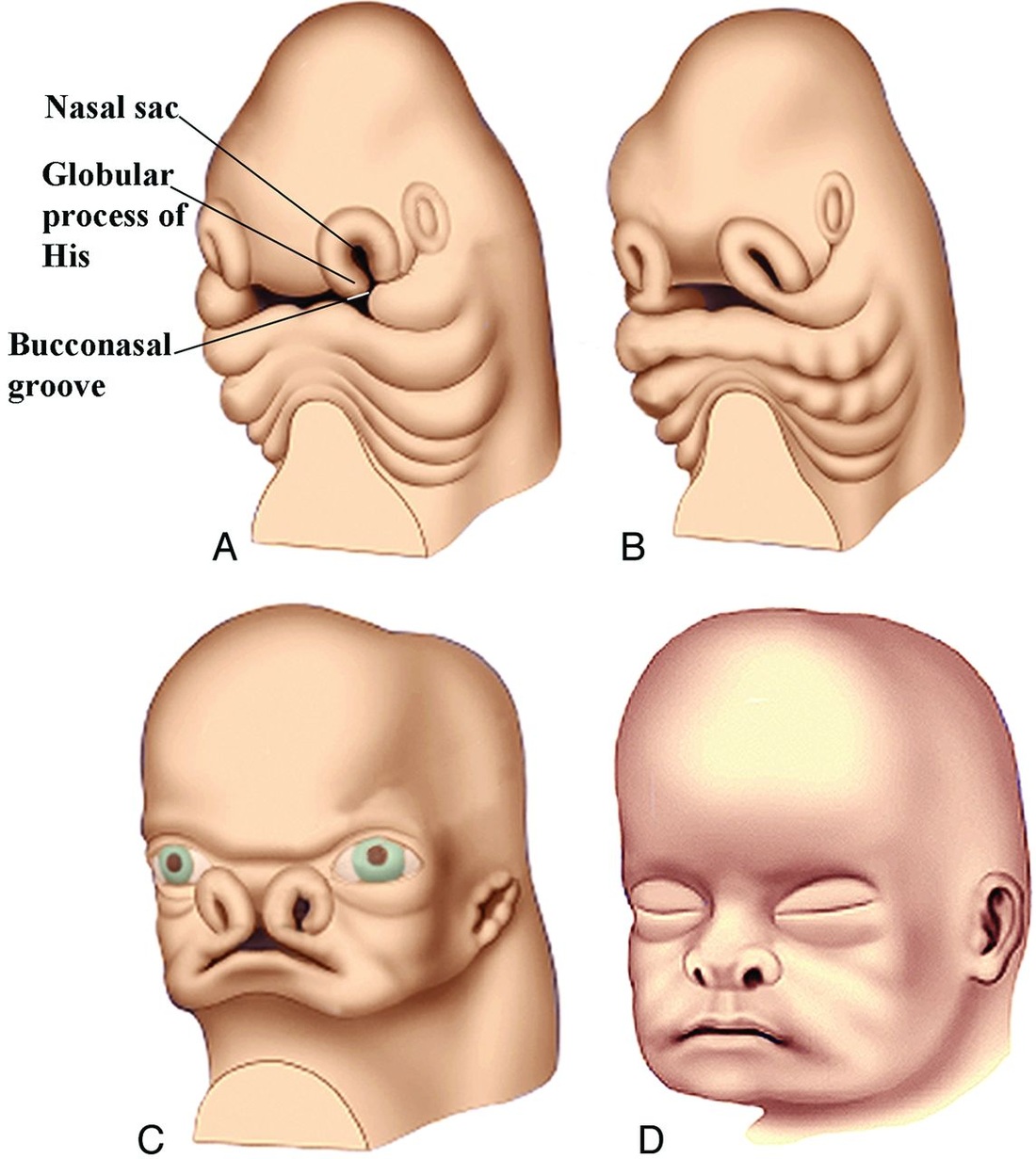
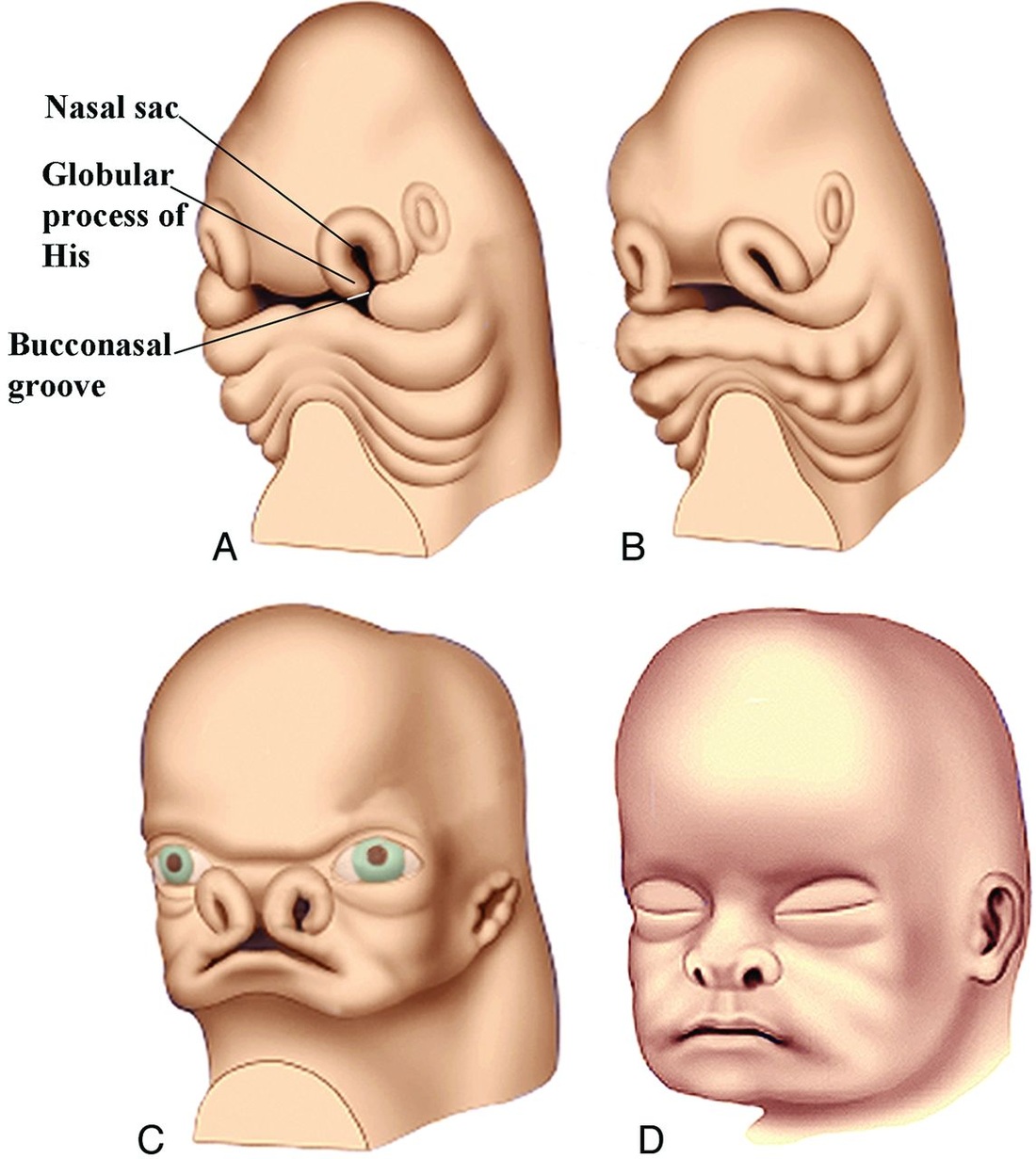
Development of the Face
Development of the Face: - 28 days after fertilization. The face develops from five processes: frontonasal, two maxillary, and two mandibular
- 33 days after fertilization. Nasal placodes, areas of thickening, appear in the frontonasal process.
- 40 days after fertilization. Maxillary processes extend toward midline. The nasal placodes also move toward the midline and fuse with the maxillary processes to form the jaw and lip.
- 48 days after fertilization. Continued growth brings structures more toward the midline.
- 14 weeks after fertilization. Contributions of each process to the adult face.
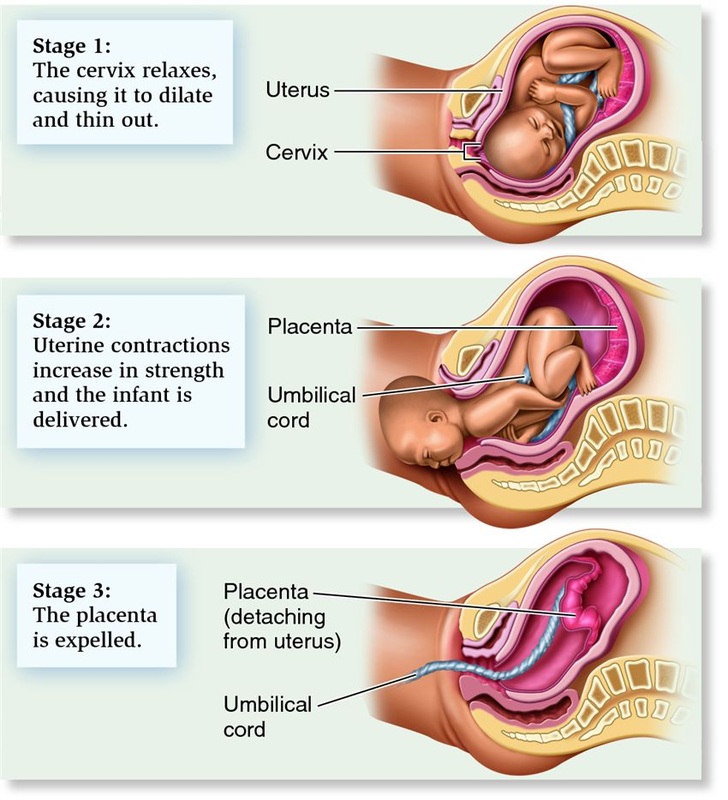
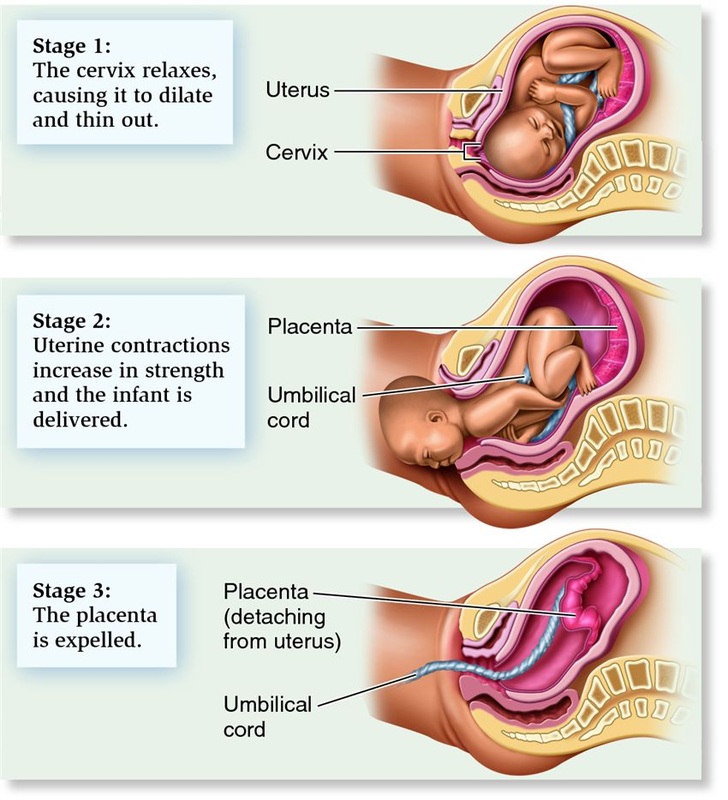
Parturition
Functions of the Reproductive System: - Production of gametes
- Fertilization
- Development and nourishment of a new individual
- Production of sex hormones
Major Organs of the Reproductive System
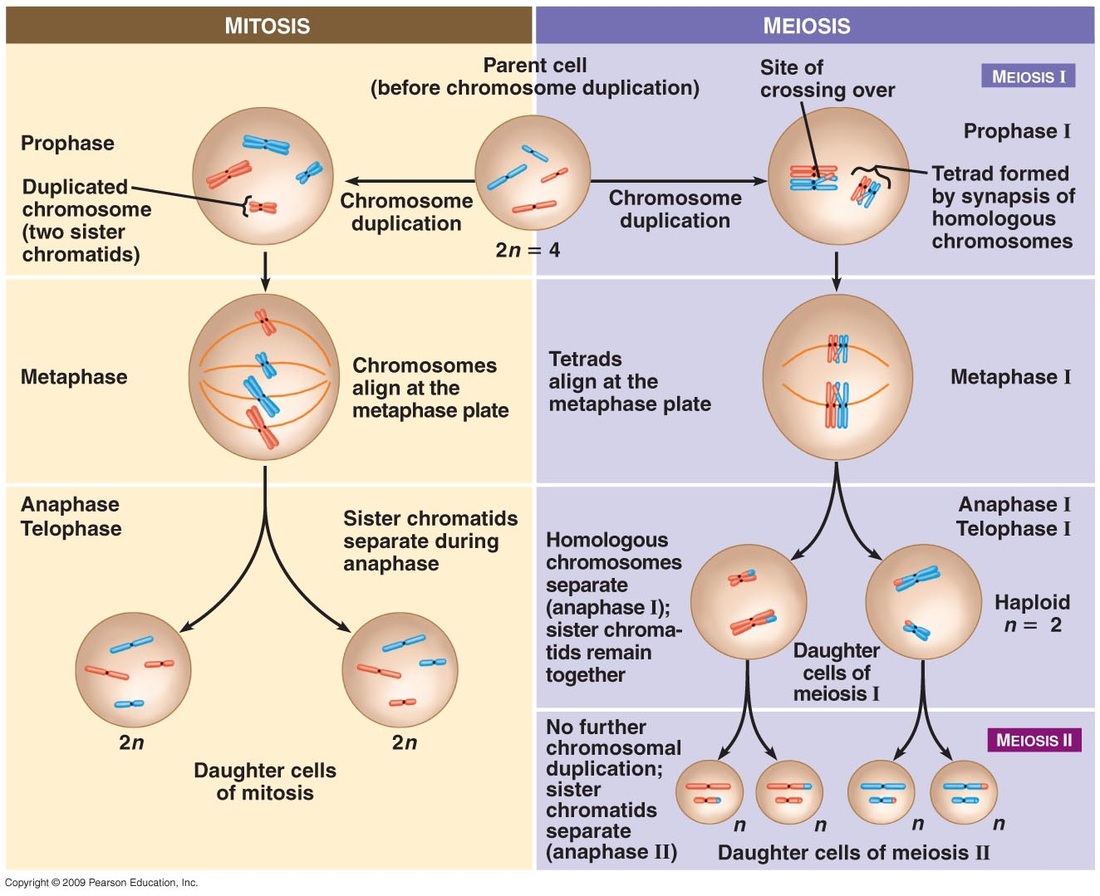
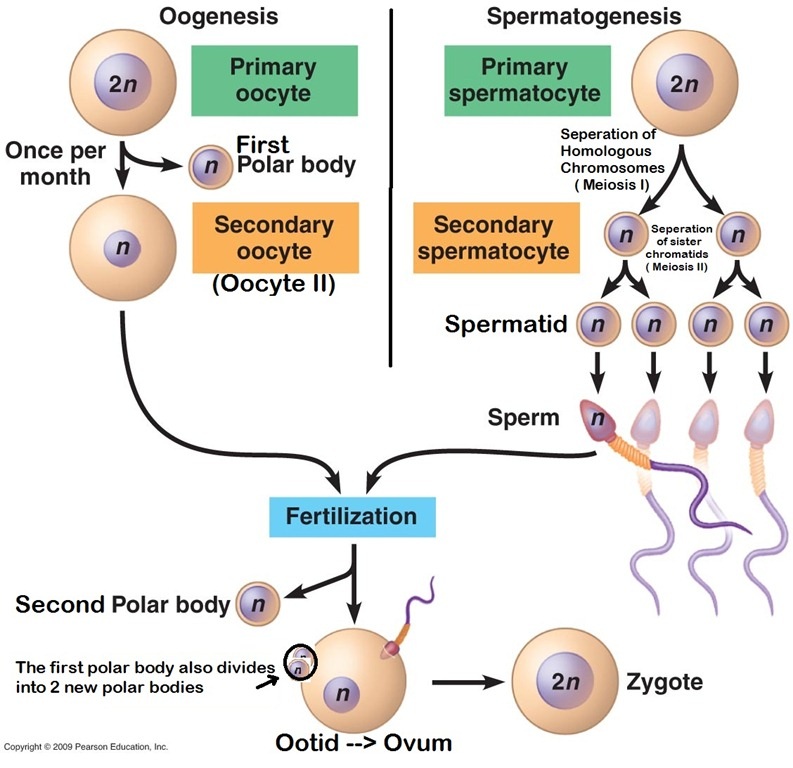
Spermatogenesis:- Spermatogonia are the cells from which sperm cells arise. The spermatogonia divide by mitosis. One daughter cell remains a spermatogonium that can divide again by mitosis. One daughter cell becomes a primary spermatocyte.
- The primary spermatocyte divides by meiosis to form secondary spermatocytes.
- The secondary spermatocytes divide by meiosis to form spermatids
- The spermatids differentiate to form sperm cells.
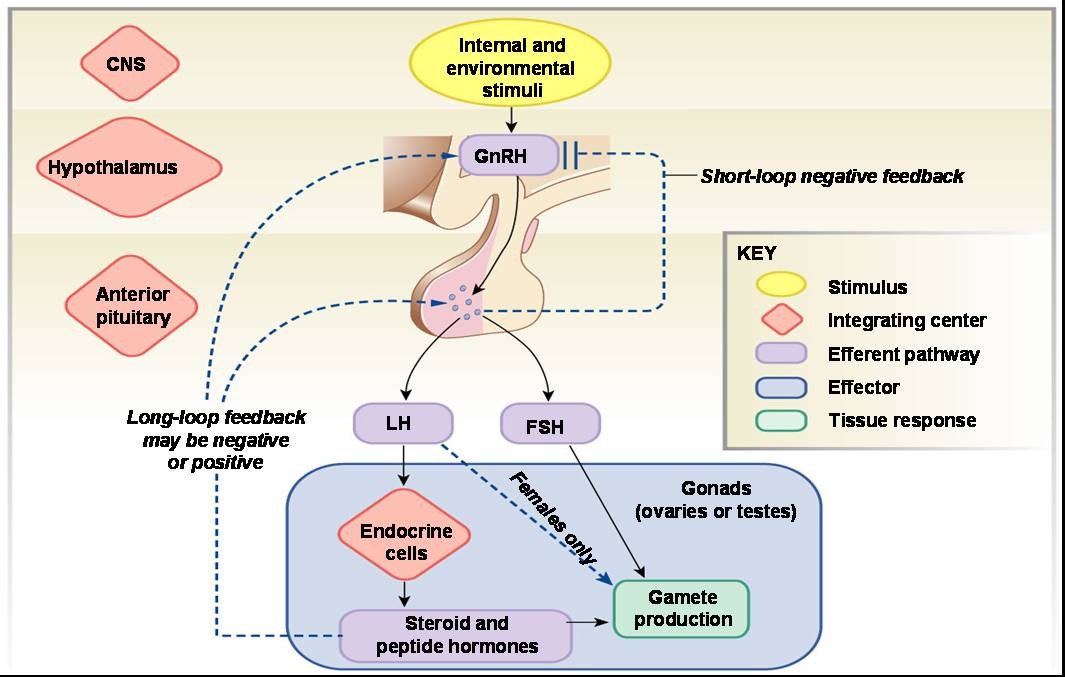
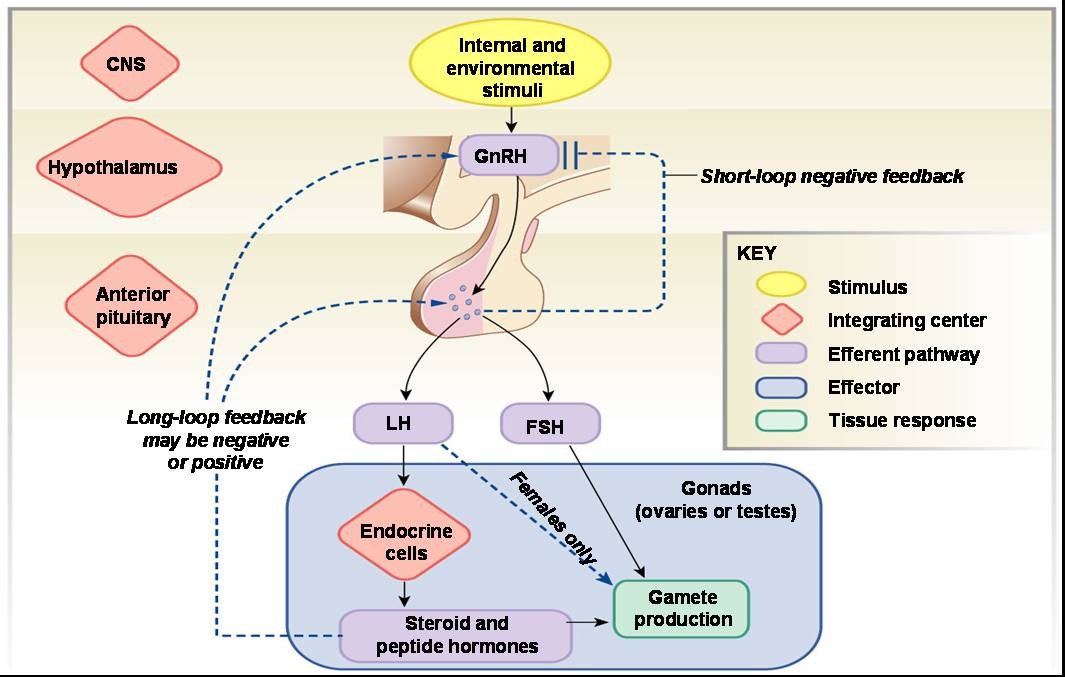
Regulation of Reproductive Hormone Secretion
Regulation of Reproductive Hormone Secretion in Males:- Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary.
- LH stimulates testosterone secretion from the interstitial cells.
- FSH stimulates sustentacular cells of the seminiferous tubules to increase spermatogenesis and to secrete inhibit.
- Testosterone has a stimulatory effect on the sustentacular cells of the seminiferous tubules, as well as on the development of sex organs and secondary sex characteristics.
- Testosterone has a negative-feedback effect on the hypothalamus and pituitary to reduce GnRH, LH, and FSH secretion.
- Inhibin has a negative-feedback effect on the anterior pituitary to reduce FSH secretion.
Maturation of the Oocyte and Follicle
- Oogonia give rise to oocytes. Before birth, oogonia multiply by mitosis. During development of the fetus, many oogonia begin meiosis, but stop in prophase I and are now called primary oocytes. They remain in this state until puberty.
- Before birth, the primary oocytes become surrounded by a single layer of granulosa cells, creating a primordial follicle. These are present until puberty.
- After puberty, primordial follicles develop into primary follicles when the granulosa cells enlarge and increase in number.
- Secondary follicles form when fluid-filled vesicles develop and thecal cells arise on the outside of the follicle.
- Mature follicles form when the vesicles create a single antrum.
- Just before ovulation, the primary oocyte completes meiosis I, creation a secondary oocyte and a nonviable polar body.
- The secondary oocyte begins meiosis II, but stops at metaphase II.
- During ovulation, the secondary oocyte is released from the ovary.
- The secondary oocyte only completes meiosis II if it is fertilized by a sperm cell. The completion of meiosis II forms an oocyte and a secondary polar body. Fertilization is complete when the oocyte nucleus and the sperm cell nucleus unite, creating a zygote.
- Following ovulation, the granulosa cells divide rapidly and enlarge to form the corpus luteum.
- The corpus luteum degenerates to form a scar, or corpus albicans.
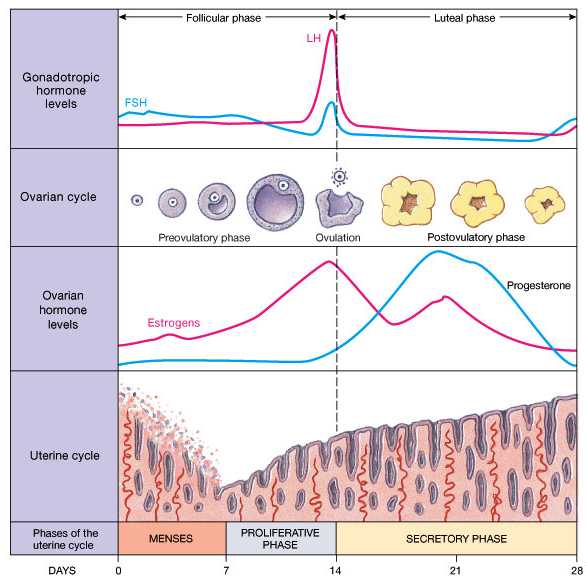
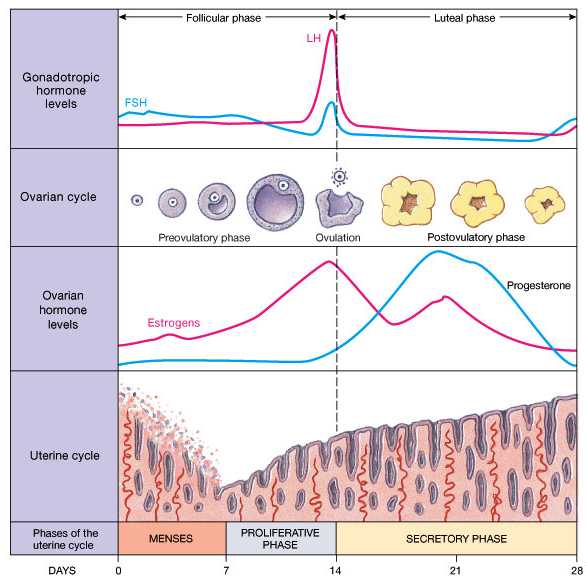
Menstrual Cycle
Over approximately 30 days, fluctuations occur in the levels of follicle-stimulating hormone FSH and luteinizing hormone LH secretion from the anterior pituitary gland and in the levels of estrogen and progesterone secretion from the ovary. In addition, changes in the ovary and changes in the endometrium of the uterus are correlated with changes in hormone secretion throughout the menstrual cycle. Ovulation occurs on about day 14.
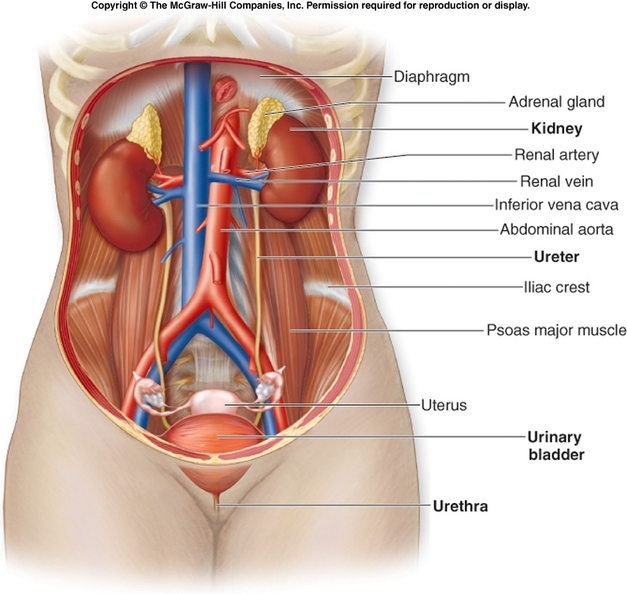
Functions of the Urinary System:- Excretion
- Regulation of blood volume and pressure
- Regulation of the concentration of solutes in the blood
- Regulation of extracellular fluid pH
- Regulation of red blood cell synthesis
- Regulation of vitamin D synthesis
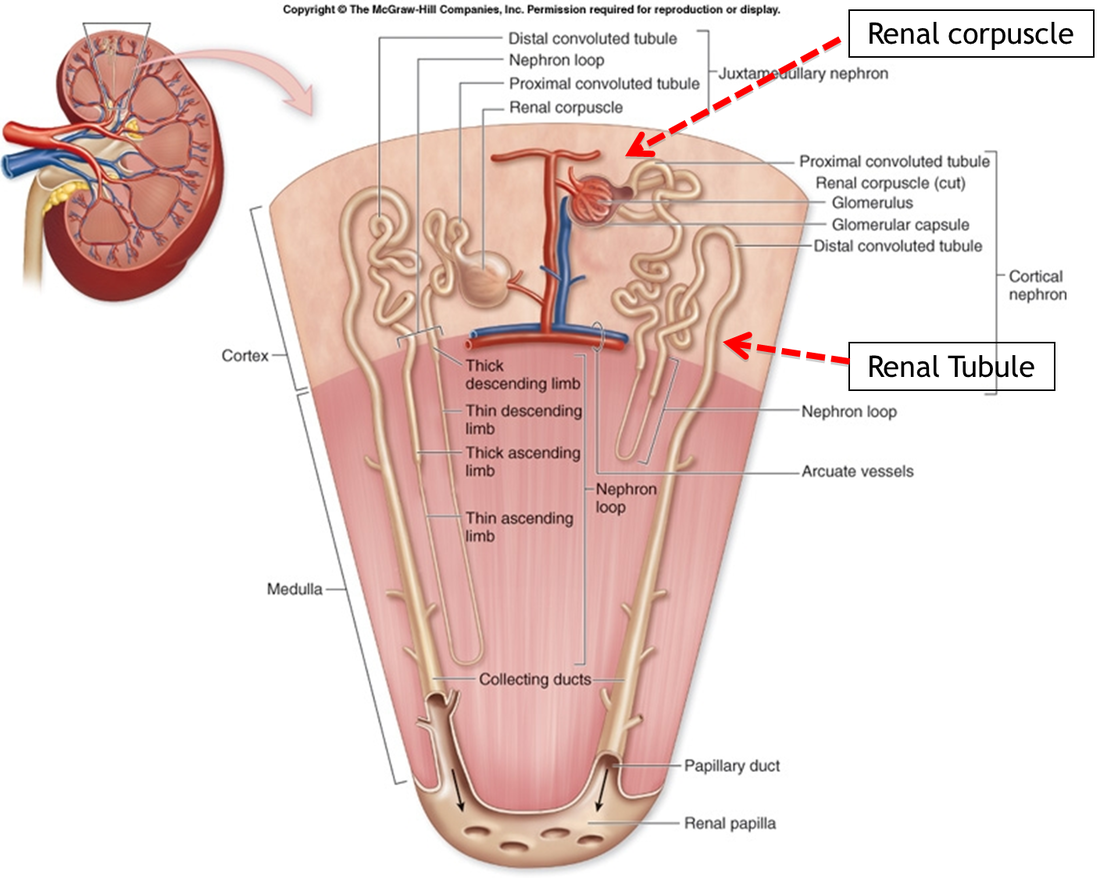
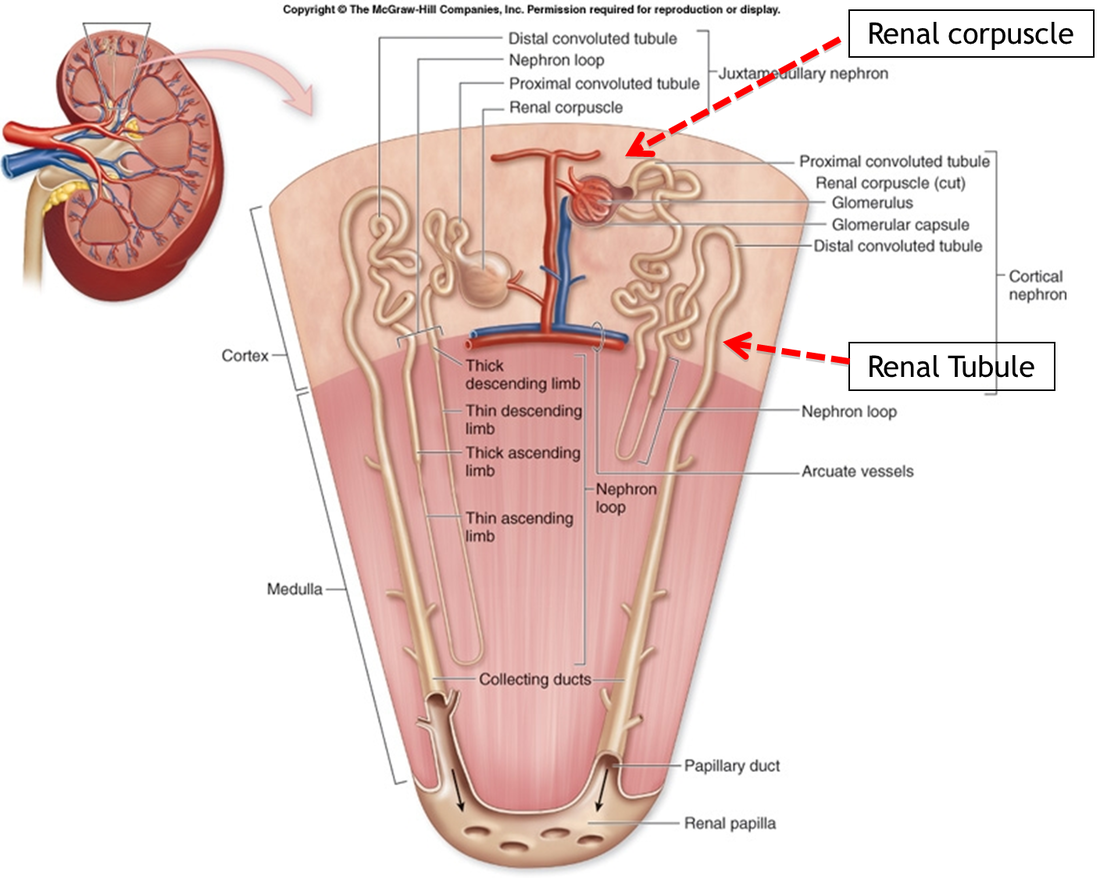
Functional Unit of the Kidney- Nephron
The functional unit of the kidney is the nephron and there are approximately 1.3 million of them in each kidney. Each nephron consists of a renal corpuscle, a proximal convoluted tubule, a loop of hence, and a distal convoluted tubule. Urine Formation: - Filtration. Filtration is the movement of materials across the filtration membrane into Bowman's capsule to form filtrate.
- Tubular Reabsorption. Solutes are reabsorbed across the wall of the nephron into the interstitial fluid by transport processes, such as active transport and cotransport. Water is reabsorbed across the wall of the nephron by osmosis. Water and solutes pass from the interstitial fluid into the peritubular capillaries.
- Tubular secretion. Solutes are secreted across the wall of the nephron into the filtrate.
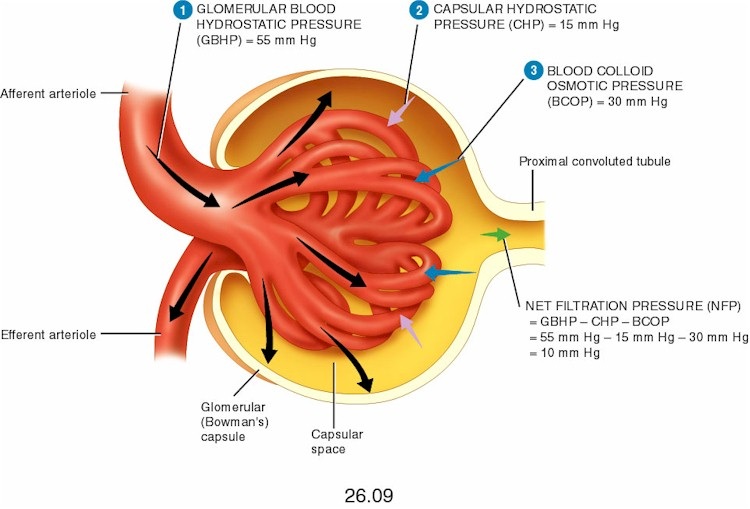
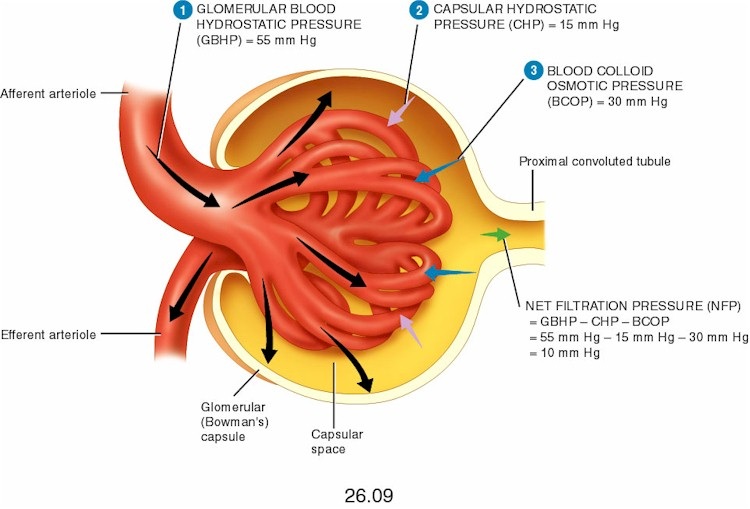
Filtration Pressure
Filtration Pressure: - Glomerular capillary pressure, the blood pressure within the glomerulus, moves fluid from the blood into Bowman's capsule.
- Capsular pressure, the pressure inside Bowman's cap sure, moves fluid from the capsule into the blood.
- Colloid osmotic pressure, produced by the concentration of blood proteins, moves fluid from Bowman's capsule into the blood by osmosis.
- Filtration pressure is equal to the glomerular capillary pressure minus the capsular and colloid osmotic pressures.
Reabsorption in the Loop of Henle: - The wall of the thin segment of the descending limb of the loop of Henle is permeable to water and, to a lesser extent, to solutes. The interstitial fluid in the medulla of the kidney and the blood in the vasa recta have a high solute concentration. Water therefore moves by osmosis from the tubule into the interstitial fluid and into the vasa recta. An additional 15% of the filtrate volume is reabsorbed. To a lesser extent, solutes diffuse from the vasa recta and interstitial fluid into the tubule.
- The thin segment of the ascending limb of the loop of Henle is not permeable to water but is permeable to solutes. The solutes diffuse out of the tubule and into the more dilute interstitial fluid as the ascending limb projects toward the cortex. The solutes diffuse into the descending vasa recta.
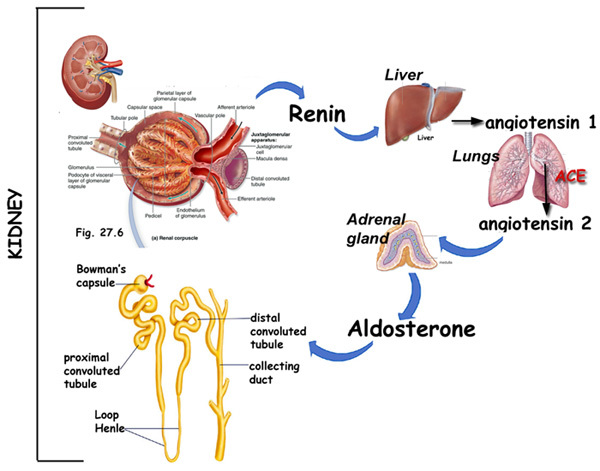
Renin and angiotensin help regulate aldosterone secretion. Renin, an enzyme secreted by cells of the juxtaglomerular apparatuses in the kidneys. Renin acts on angiotensinogen, a plasma protein produced by the liver, and converts it to angiotensin I. Angiotensin I is rapidly converted to a smaller peptide called angiotensin II by angiotensin-converting enzyme (ACE). Angiotensin II acts on the adrenal cortex, causing it to secrete aldoesterone.
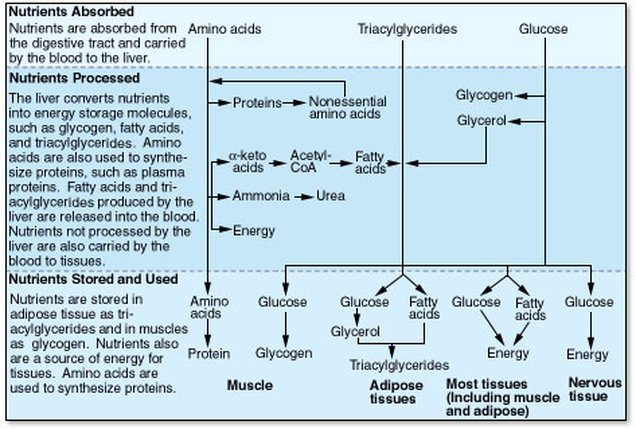
- Nutrients are the chemicals taken into the body that provide energy and building blocks for new molecules.
- Essential nutrients are nutrients that must be ingested because the body cannot manufacture them- or it cannot manufacture them in adequate amounts.
- Carbohydrates include monosaccharides, disaccharides, and polysaccharides. Although most of the carbohydrates we ingest are derived from plants, lactose is derived from animals. The most common monosaccharides in the diet are glucose and fructose. Plants capture energy from sunlight and use that energy to produce glucose, which can be found in vegetables, fruits, molasses, honey, and syrup. Fructose is most often derived from fruits and berries.
- Complex carbohydrates are large polysaccharides, which are composed of long chains of glucose. Examples are starch, glycogen, and cellulose, which differ from one another in the arrangement of the glucose molecules and the structure of the chemical bonds holding them together. Starch is an energy-storage molecule in plants and is found primarily in vegetables, fruits, and grains. Glycogen is an energy-storage molecule in animals and is located primarily in muscle and in the liver. cellulose forms plant cell walls.
- Lipids include triglycerides, steroids, phospholipids, and fat-soluble vitamins. Trigylcerides, are the most common type of lipid in the diet, accounting for about 95% of the total lipid intake.
- Proteins are chains of amino acids. They are found in most of the plant and animal products we eat. Proteins in the body are constructed of 20 different kinds of amino acids, which are divided into two groups: essential amino acids and nonessential amino acids. Essential amino acids are those the body cannot synthesize, so they must be obtained in the diet. The nine essential amino acids are histidine, isoleucine, leucine, lysine, methionine, phenylalanine, tryptophan, and valine. Nonessential amino acids are necessary to contract our proteins but do not necessarily need to be ingested, since they can by synthesized from the essential amino acids.
- Vitamins are organic molecules that exist in minute quantities in food and are essential to normal metabolism. Essential vitamins cannot be produced by the body and must be obtained through the diet.
- Minerals are inorganic nutrients that are essential for normal metabolic functions. people ingest minerals alone or in combination with organic molecules.
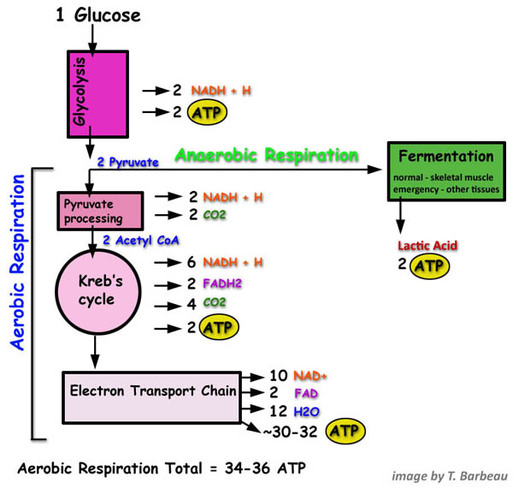
Aerobic Respiration: - Glycolysis in the cytoplasm converts glucose to two pyretic acid molecules and produces two ATP and two NADH. The NADH can go to the electron-transport chain in the inner mitochondrial membrane.
- The two pyruvic acid molecules produced in glycolysis are converted to two acetyl-CoA molecules, producing two CO2 and two NADH can go to the electron-transport chain.
- The two acetyl-CoA molecules enter the citric acid cycle, which produces four Co2, six NADH, two FDH, and two ATP. The NADH and FADH2 can go to the electron-transport chain.
- The electron-transport chain uses NADH and FADH2 to produce 34 ATP. This process requires O2, which combines with H+ to form H2O.
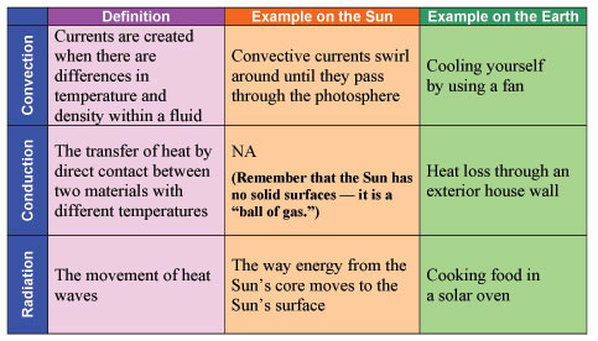
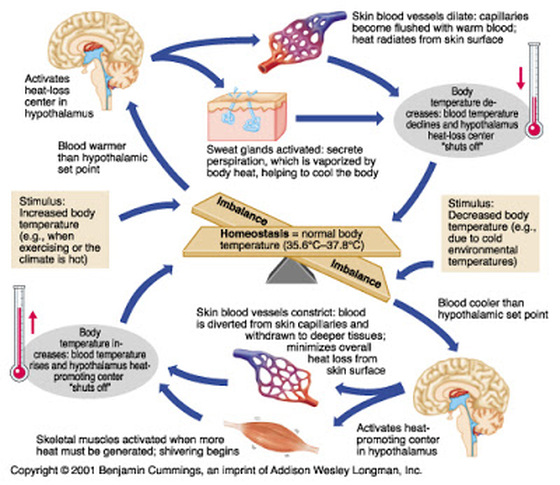
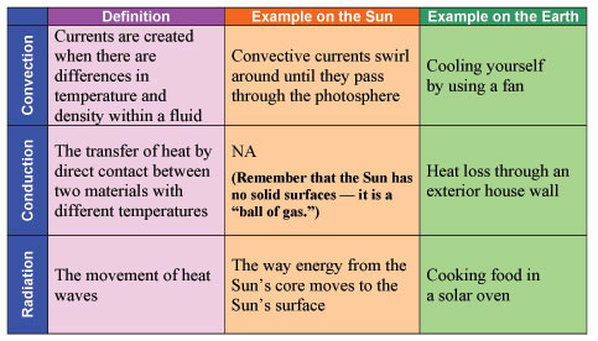
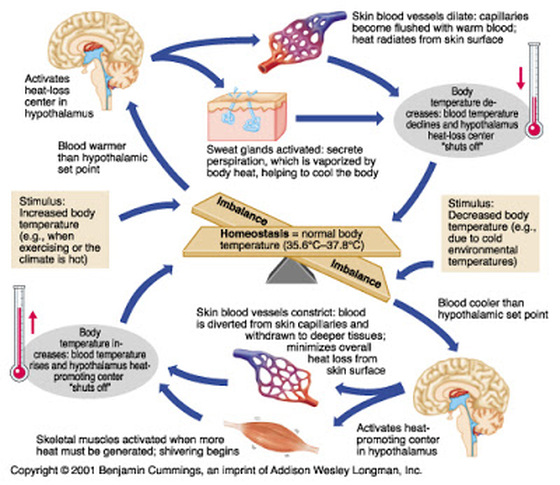
Heat Exchange
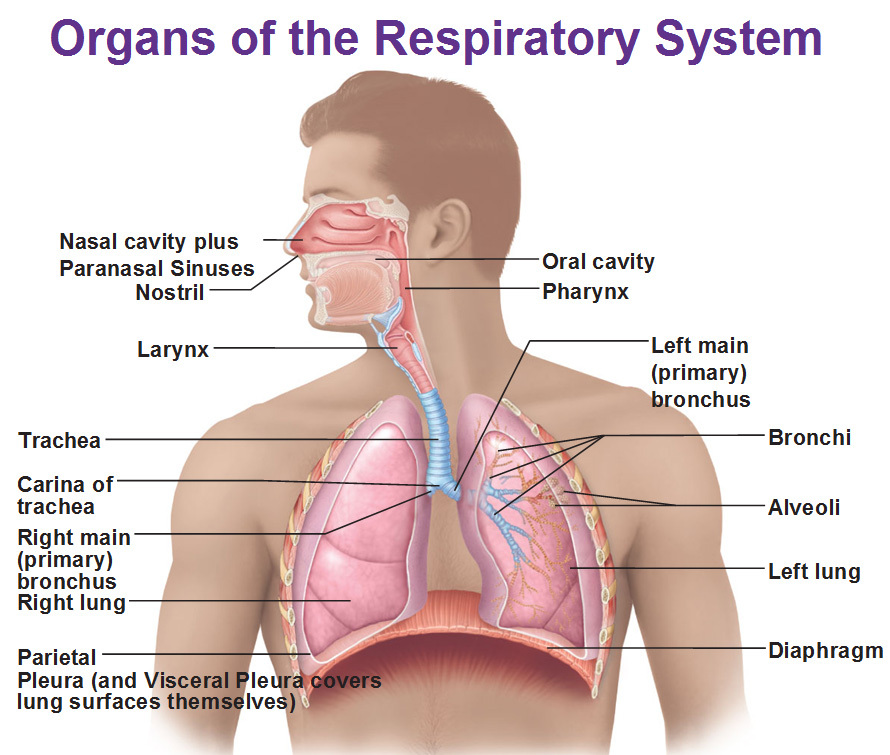
Functions of the Respiratory System:- Regulation of blood pH
- Voice production
- Olfaction
- Innate immunity
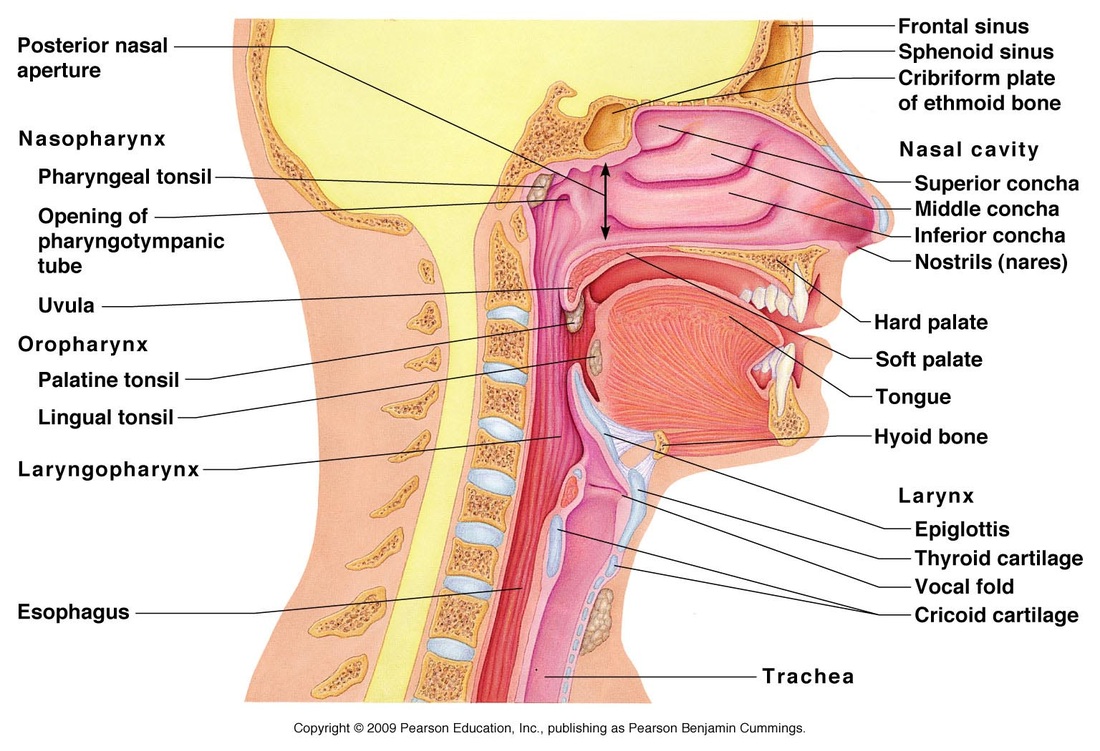
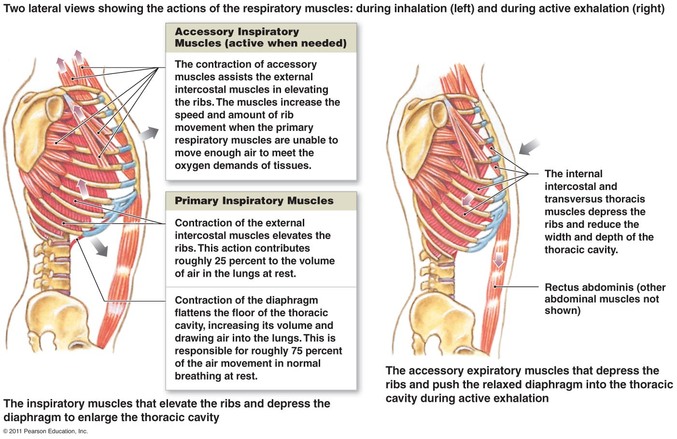
The Respiratory System is divided into the upper and lower respiratory tract. The upper respiratory tract includes: the external nose, the nasal cavity, the pharynx, and associated structures. The lower respiratory tract includes: the larynx, the trachea, the bronchi, and the lungs. The pharynx is the common passageway for both the respiratory and the digestive system. Air from the nasal cavity and air, food, and water from the mouth pass through the pharynx. Inferiorly, the pharynx leads to the rest of the rest of the respiratory system through the opening into the larynx and to the digestive system through the esophagus. The pharynx can be divided into three regions: the nasopharynx, the oropharynx, and the laryngopharynx.
The larynx is located in the anterior throat and extends from the base of the tongue to the trachea. It is a passageway for air between the pharynx and the trachea. The larynx consists of an outer casing of nine cartilages connected to one another by muscle and ligaments.
The trachea, or windpipe, is a membranous tube attached to the larynx. It consists of connective tissue and smooth muscle, reinforced with 16-20 C-shaped pieces of hyaline cartilage.
The trachea divides into the left and right main bronchi, or primary bronchi, each of which connects to a lung. The left main bronchus is more horizontal than the right main bronchus because it is displaced by the heart. Foreign objects that enter the trachea usually lodge in the right main bronchus, because it is wider, shorter, and more vertical than the left main bronchus and is more in direct line with the trachea. The main bronchi extend from the trachea to the lungs.
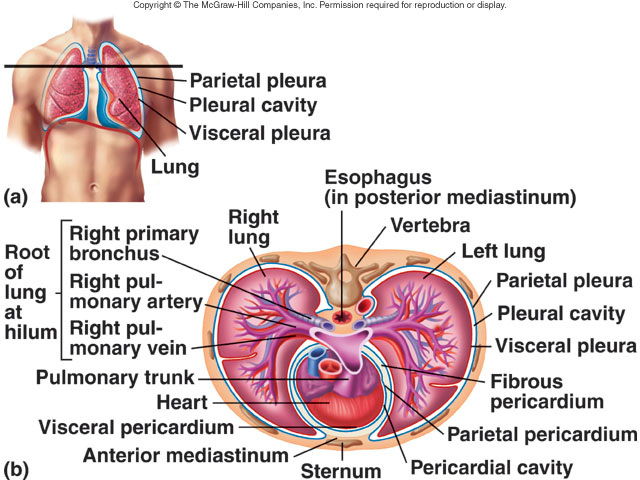
The lungs are the principal organs of respiration. Each lung is cone-shaped, with its base resting on the diaphragm and its apex extending superiorly to a point about 2.5 cm above the clavicle. The right lung has three lobes, called the superior, middle and inferior lobes. The left lung has two lobes, called the superior and inferior lobes. The lobes of the lungs are separated by deep, prominent fissures on the lung surface. Pleural Cavities:
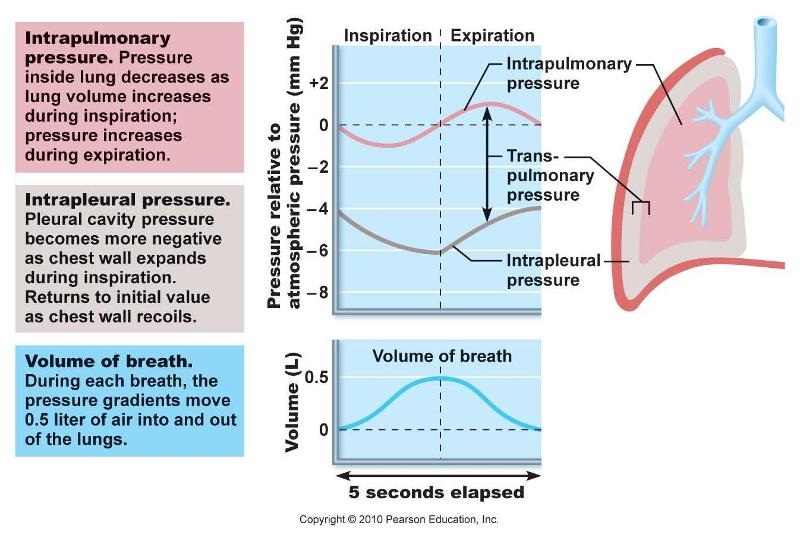
The lungs are contained within the thoracic cavity. In addition, each lung is surrounded by a separate pleural cavity. Each pleural cavity is lined with a serous membrane called the pleura. The pleura consists of a parietal and a visceral part. The parietal pleura, which lines the walls of the thorax, diaphragm, and mediastinum, is continuous with the visceral pleura, which covers the surface of the lung. Respiratory Volumes: - Tidal Volume- the volume of air inspired or expired with each breath. At rest, quiet breathing results in a tidal volume of about 500 mL.
- Inspiratory reserve volume- the amount of air that can be inspired forcefully beyond the resting tidal volume. (about 3000 mL)
- Expiratory reserve volume- the amount of air that can be expired forcefully beyond the resting tidal volume (about 1100 mL)
- Residual volume- the volume of air still remaining in the respiratory passages and lungs after maximum expiration (about 1200 mL)
Respiratory Capacities: - Functional residual capacity- the expiratory reserve volume plus the residual volume. This is the amount of air remaining in the lungs at the end of a normal expiration (about 2300 mL at rest)
- Inspiratory capacity- the tidal volume plus the inspiratory reserve volume. This is the amount of air a person can inspire maximally after a normal expiration (about 3500 mL)
- Vital capacity- the sum of the inspiratory reserve volume, the tidal volume, and the expiratory reserve volume. It is the maximum volume of air that a person can expel from the respiratory tract after a maximum inspiration (about 4600 mL)
- Total lung capacity- the sum of the inspiratory and expiratory reserves and the tidal and residual volumes (about 5800 mL). The total lung capacity is also equal to the vital capacity plus the residual volume.
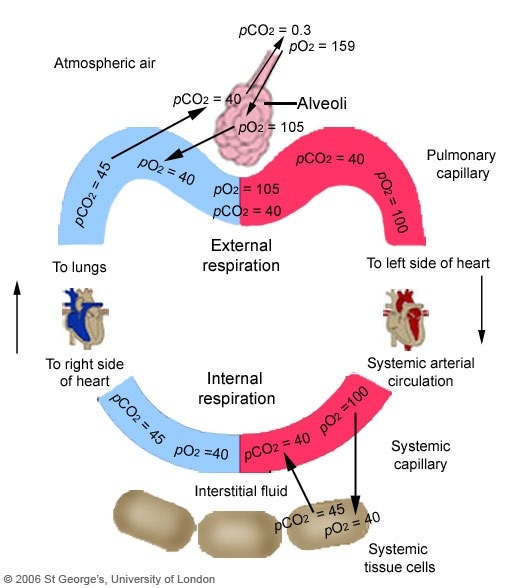
Gas Exchange:- Oxygen diffuses into the arterial ends of pulmonary capillaries, and CO2 diffuses into the alveoli because of differences in partial pressures.
- As a result of diffusion at the venous ends of pulmonary capillaries, the Po2 in the blood is equal to the Po2 in the alveoli, and the Pco2 in the blood is equal to the Pco2 in the alveoli.
- The Po2 of blood in the pulmonary veins is less than in the pulmonary capillaries because of mixing with deoxygenated blood from veins draining the bronchi and bronchioles.
- Oxygen diffuses out of the arterial ends of tissue capillaries, and CO2 diffuses out of the tissue because of differences in partial pressures.
- As a result of diffusion at the venous ends of tissue capillaries, the Po2 in the blood is equal to the Po2 in the tissue, and the Pco2 in the blood is equal to the Pco2 in the tissue.
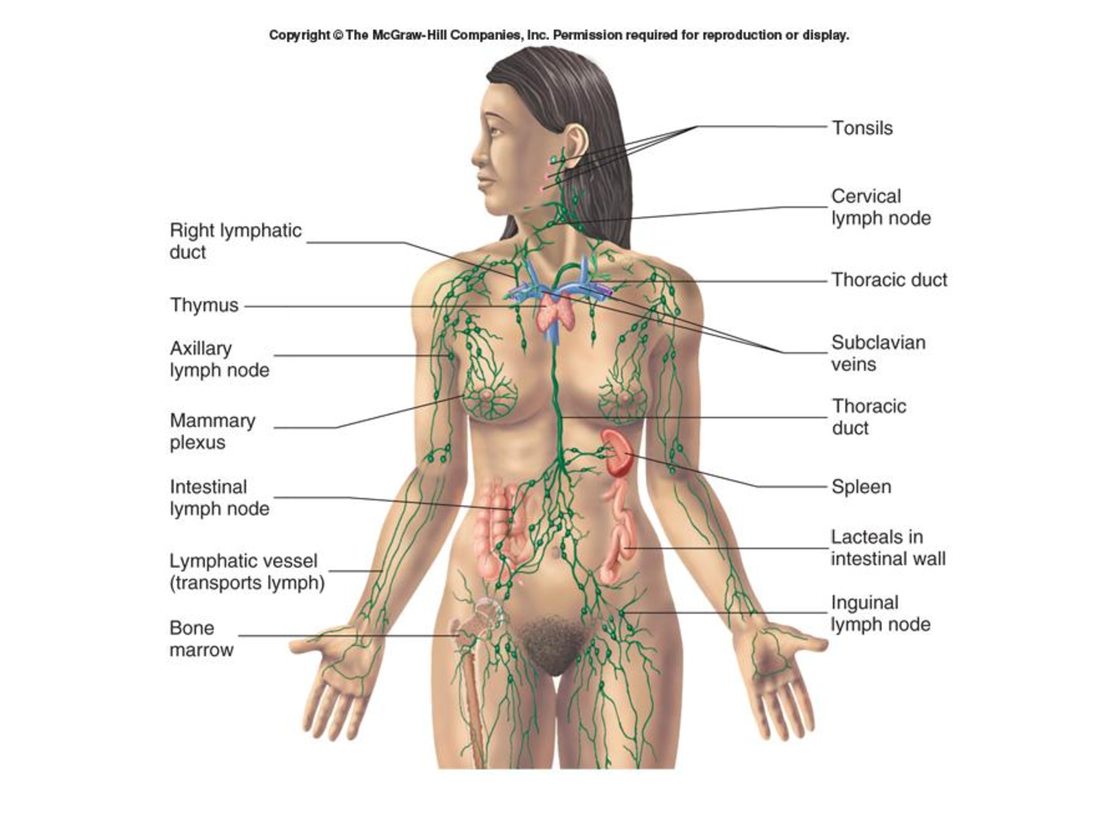
Functions of the Lymphatic System: - Fluid Balance
- Fat absorption
- Defense
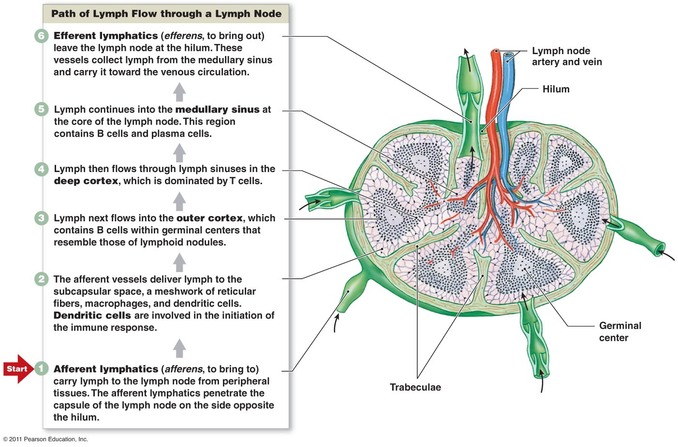
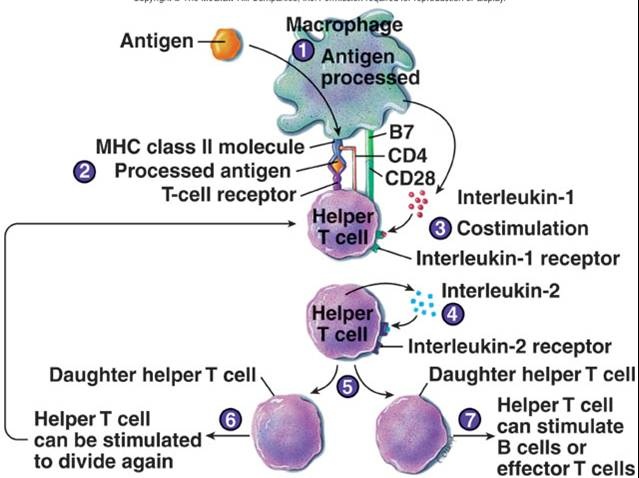
Overview of the Lymphatic System:- Lymphatic capillaries remove fluid from tissues. The fluid becomes lymph.
- Lymph flows through lymphatic vessels, which have valves that prevent the back flow of lymph.
- Lymph nodes filter lymph and are sites where lymphocytes respond to infections.
- Lymph enters the thoracic duct or the right lymphatic duct.
- Lymph enters the blood.
- Lacteals in the small intestine absorb fats, which enter the thoracic duct.
- Chyle, which is lymph containing fats, enters the blood.
- The spleen filters blood and is a site where lymphocytes respond to infections.
- Lymphocytes (pre-B and pre-T cells) originate from stem cells in the red bone marrow. The pre-B cells become mature B cells in the red bone marrow and are released into the blood. The pre-T cells enter the blood and migrate to the thymus.
- The thymus is where pre-T cells derived from red bone marrow increase in number and become mature T cells that are released into the blood.
- B cells and T cells from the blood enter and populate all lymphatic tissues. These lymphocytes can remain in tissues or pass through them and return to the blood. B cells and T cells can also respond to infections by dividing and increasing in number. Some of the newly formed cells enter the blood and circulate to other tissues.
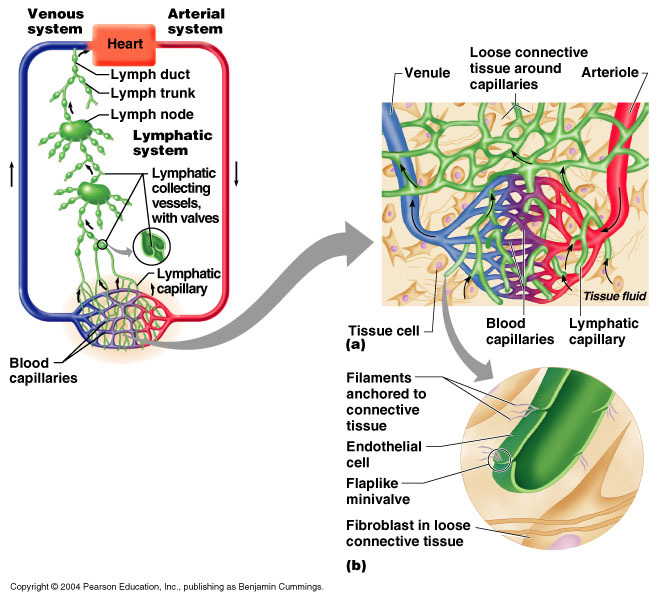
Proliferation of Helper T Cells: - Antigen-presenting cells, such as macrophages, phagocytize, process, and display antigens on the cell's surface.
- The antigens are bound to MHC class II molecules, which present the processed antigen to the T-cell receptor of the helper T cell.
- Costimulation results from interleukin-1, secrete by the macrophage, and the CD4 glycoprotein of the helper T cell.
- Interleukin-1 stimulates the helper T cell to secrete interleukin-2 and to produce interleukin-2 receptors.
- The helper T cell stimulates itself to divide when interleukin-2 binds to interleukin-2 receptors.
- The "daughter" helper T cells resulting from this division can be stimulated to divide again if they are exposed to the same antigen that stimulated the "parent" helper T cell. This greatly increases the number of helper T cells.
- The increased number of helper T cells can facilitate the activation of B cells or effector T cells.
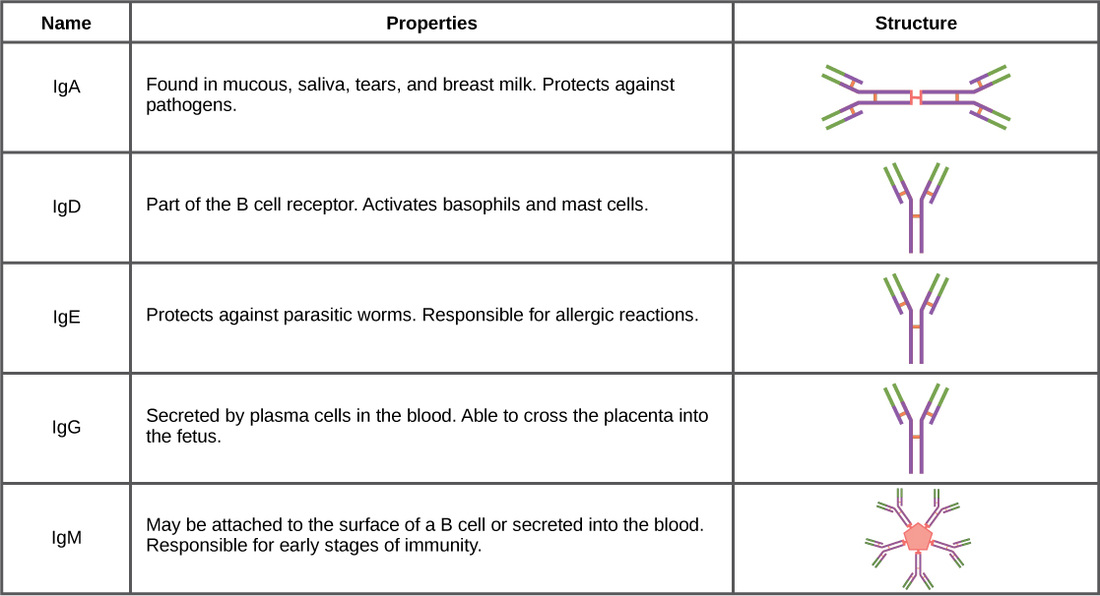
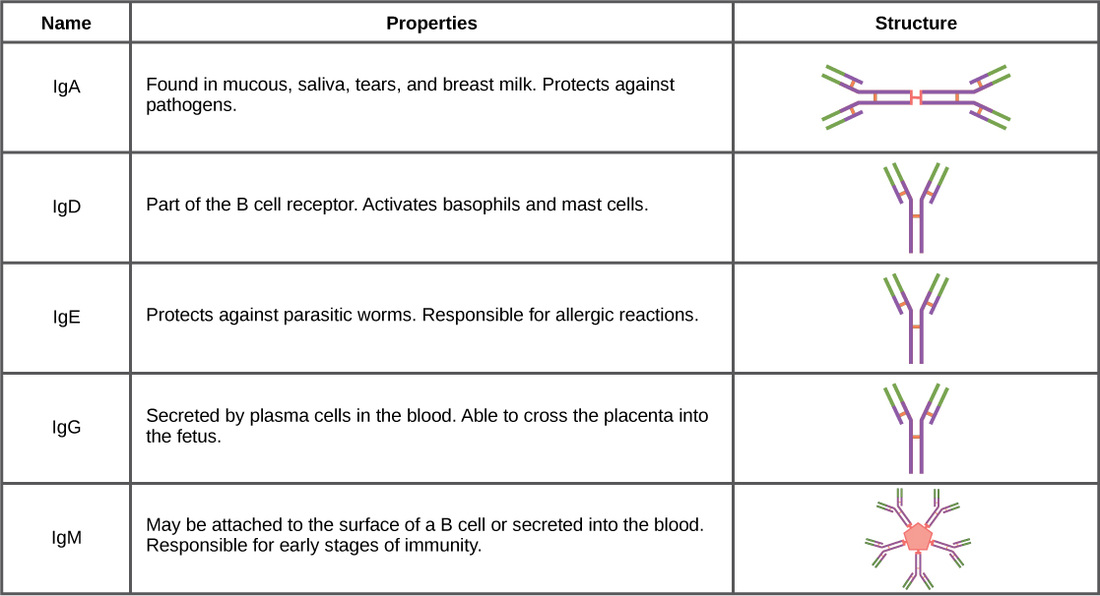
Classes of Antibodies and their functions
Proliferation of Cytotoxic T Cells:- An MHC class I molecule displays an antigen, such as viral protein, on the surface of a target cell.
- The activation of cytotoxic T cell begins when the T-cell receptor binds to the MHC class I/antigen complex.
- There is costimulation of the cytotoxic T cell by CD8 and other surface molecules.
- There is costimulation by cytokines, such as interleukin-2, released from helper T cells.
- The activated cytotoxic T cell divides, the resulting daughter cell divide, and so on, eventually pro ducting many cytotoxic T cells.
The circulatory system has five functions:- Carries Blood
- Exchanges nutrients, waste products, and gases with tissues
- Transports substances
- Helps regulate blood pressure
- Directs blood flow to the tissues
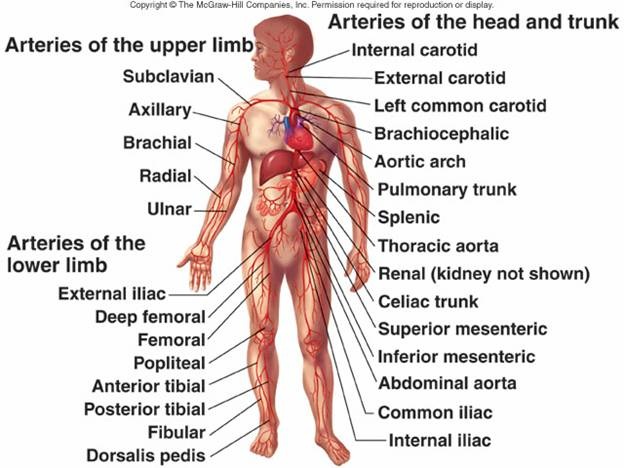
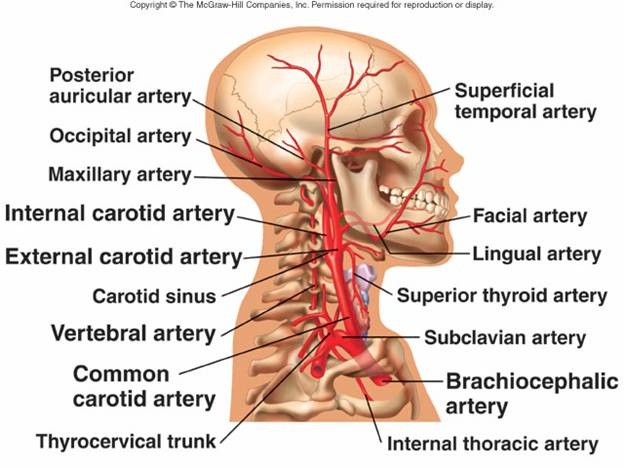
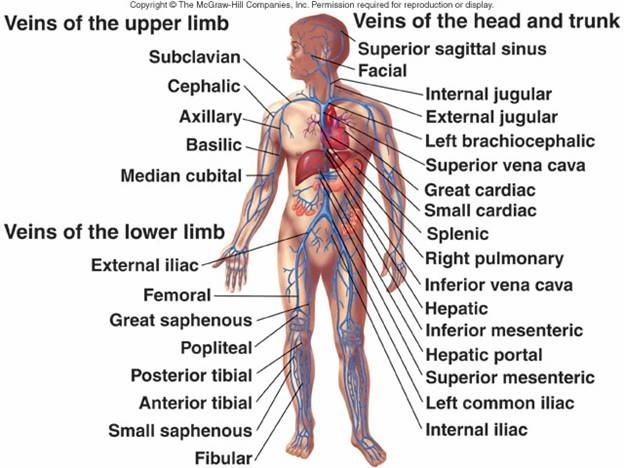
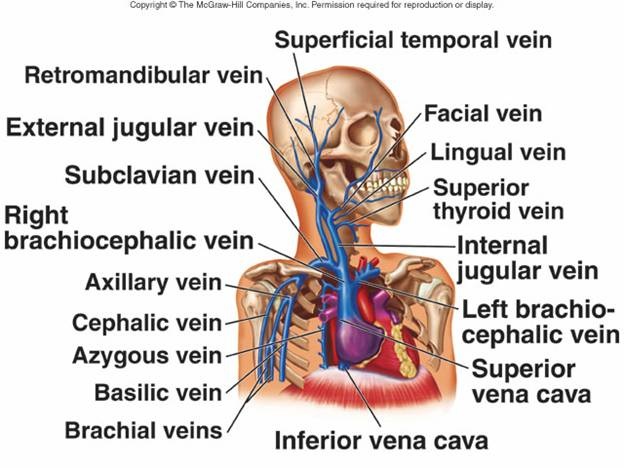
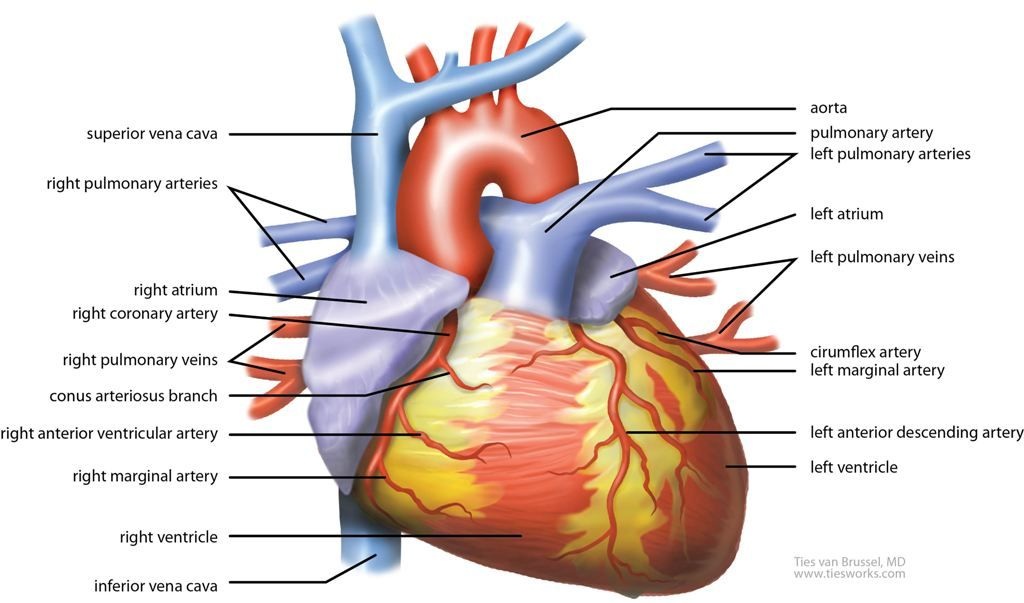
The three main types of blood vessels are arteries, capillaries, and veins.
Arteries- carry blow away from the heart, usually the blood is oxygen-rich. Blood is pumped from the ventricles of the heart into large, elastic arteries, which branch repeatedly to form progressively smaller arteries. As they become smaller, the artery walls undergo a gradual tradition from having more elastic tissue than smooth muscle to having more smooth muscle than elastic tissue. The arteries are normally classified as elastic, muscular arteries, or arterioles, although they form a continuum from the largest to the smallest branches.
Blood flows from arterioles into capillaries, where exchange occurs between the blood and the tissue fluid. Capillaries have thinner walls than do arteries. Blood flows through them more slowly, and there are far more of them than of any other blood vessel type.
From the capillaries, blood flows into veins. Veins carry blood toward the heart; usually, the blood is oxygen-poor. Compared to arteries, the walls of veins are thinner and contain less elastic tissue and fewer smooth muscle cells. Starting at capillaries and proceeding toward the heart, small diameter veins come together to form larger-diameter veins, which are fewer in number. Veins increase in diameter and decrease in number as they progress toward the heart, and their walls increase in thickness. Veins may be classified as venues, small veins, medium-sized veins, or large veins.
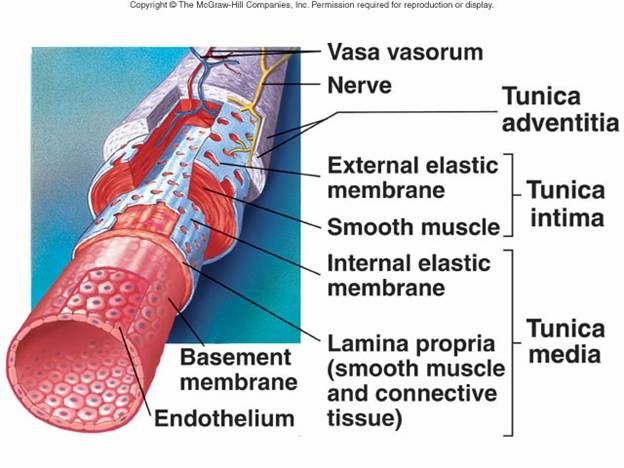
Except in capillaries and venues, blood vessel walls consist of three layers, or tunics. From the inner to the outer wall, the tunics are 1.) the tunica intima, 2.) the tunica media, and 3.) the tunica adventitia, or tunica externa.
Measuring Blood Pressure:- When the cut pressure is high enough to keep the brachial artery closed, no blood flows through it, and no sound is heard.
- When cuff pressure decreases and is no longer ale to keep the brachial artery closed, blood is pushed through the partially opened brachial artery, producing turbulent blood flow and a sound. Systolic pressure is the pressure at which a sound is first heard.
- As cuff pressure continues to decrease, the brachial artery opens even more during systole. At first, the artery is closed during diastole, but as cuff pressure continues to decrease, the brachial artery partially opes during diastole. Turbulent blood flow during systole produces Korotkoff sounds, although the pitch of the sounds changes as the artery becomes more open.
- Eventually the cuff pressure decreases below the pressure in the brachial artery, and it remains open during systole and diastole. Nonturbulent flow is reestablished, and no sounds are heard. Diastolic pressure is the pressure at which the sound disappears.
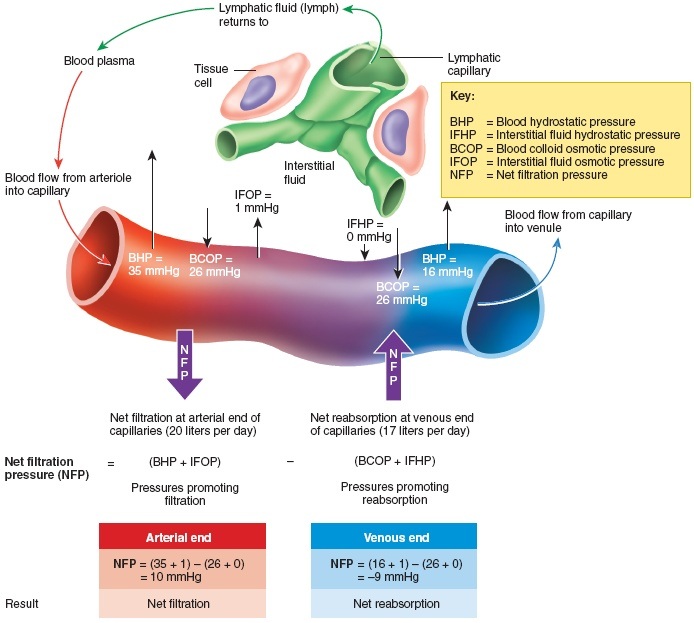
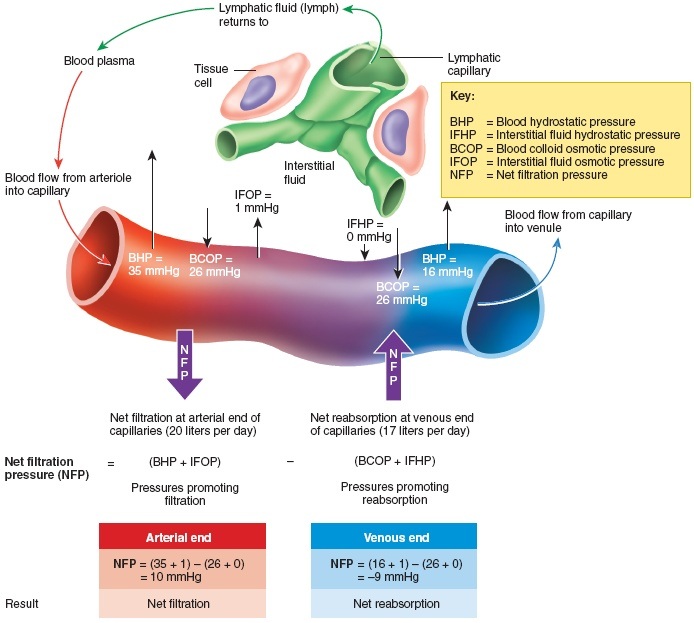
Capillary Exchange
Capillary Exchange:- At the arterial end of the capillary, the movement of fluid out of the capillary due to blood pressure is greater than the movement of fluid into the capillary due to osmosis.
- At the venous end of the capillary, the movement of fluid into the capillary due to osmosis is greater than the movement of fluid out of the capillary due to blood pressure.
- Approximately nine-tenths of the fluid that leaves the capillary at its arterial end reenters the capillary at its venous end. About one-tenth of the fluid passes into the lymphatic capillaries.
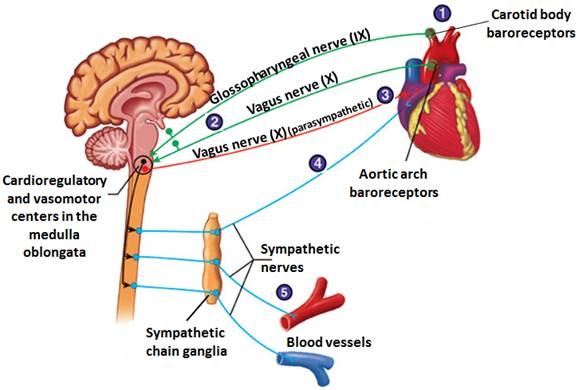
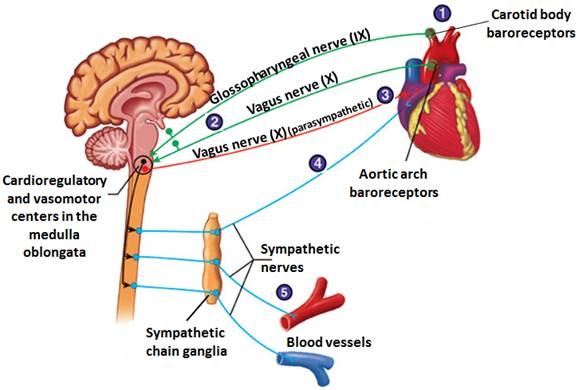
Baroreceptor Reflex Mechanism
Baroreceptor Reflex Mechanism:- Baroreceptors in the carotid sinus and aortic arch monitor blood pressure.
- Sensory nerves conduct action potentials to the cardioregulatory and vasomotor centers in the medulla oblongata.
- Increased parasympathetic stimulation of the heart decreases the heart rate.
- Increased sympathetic stimulation of the heart increases the heart rate and stroke volume.
Chemoreceptor Reflex Mechanism:- Chemoreceptors in the carotid and aortic bodies monitor blood O2, CO2, and pH.
- Chemoreceptors in the medulla oblongata monitor blood CO2 and pH.
- Decreased blood O2, increased CO2, and decreased pH decrease parasympathetic stimulation of the heart, which increases the heart rate.
- Decreased blood O2, increased CO2, and decreased pH increase sympathetic stimulation of the heart, which increases the heart rate and stroke volume.
- Decreased blood O2, increased CO2, and decreased pH increase sympathetic stimulation of blood vessels, which increases vasoconstriction.
Functions of the Heart: - Generating blood pressure.
- Routing blood.
- Ensuring one-way blood flow.
- Regulating blood supply.
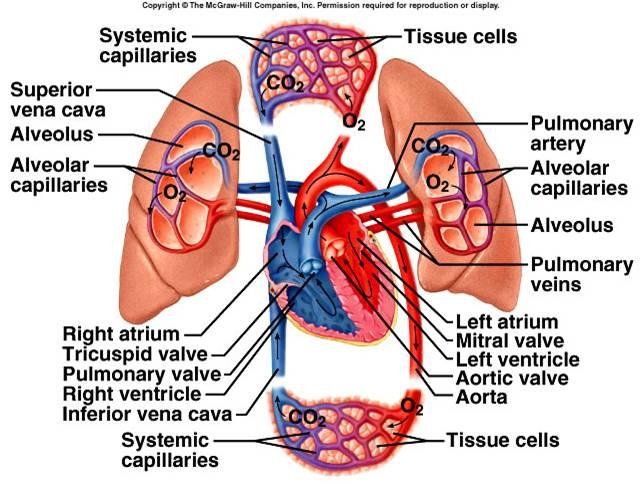
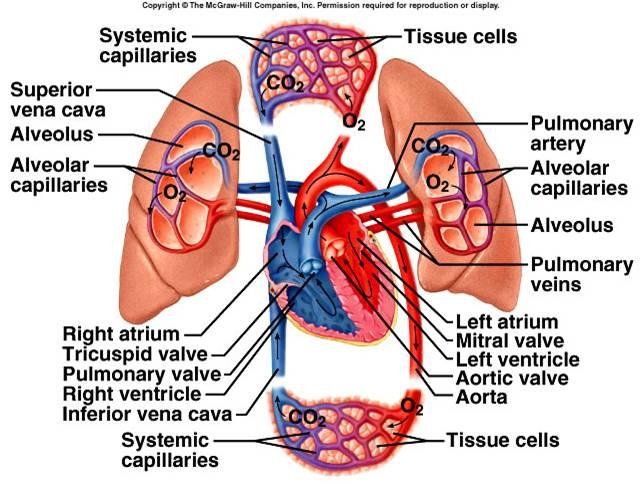
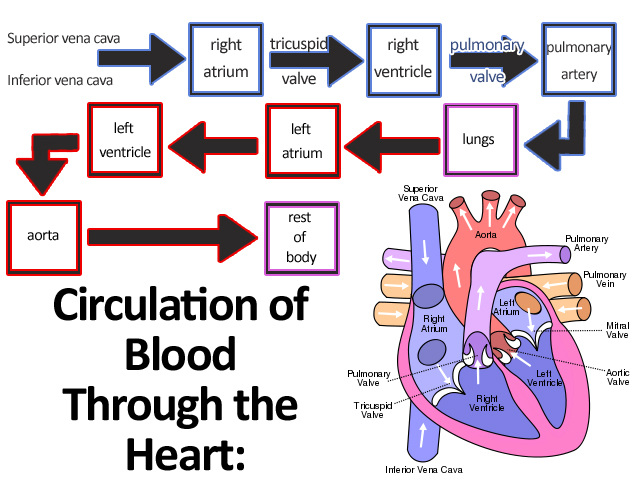
Overview of Circulatory System
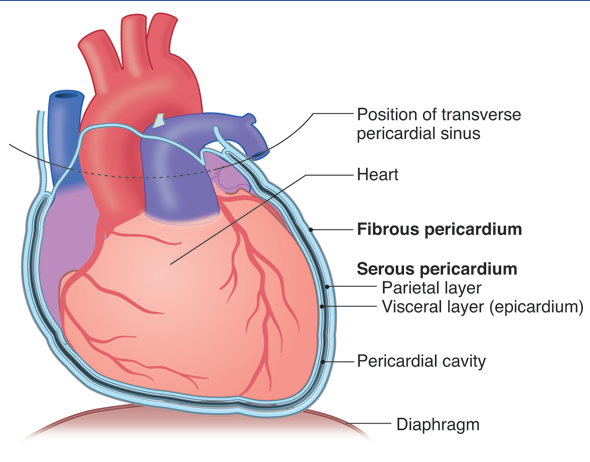
The right side of the heart pumps blood to the lungs and back tot he left side of the heart through vessels of the pulmonary circulation. The left side of the heart pumps blood to all other tissues of the body and back to the right side of the heart through vessels of the systemic circulation. Pericardium:
The heart lies in the pericardial cavity. The pericardial cavity is formed by the pericardium, or pericardial sac, tissues that surround the heart and anchor it within the mediastinum. The pericardium consists of two laters: the fibrous pericardium and the serous pericardium. The portion of the serious pericardium lining the fibrous pericardium is the parietal pericardium, whereas the portion covering the heart surface is the visceral pericardium, or epicardium. The parietal and visceral pericardia are continuous with each other where the great vessels enter or leave the heart. The pericardial cavity, located between the visceral and parietal pericardia, is filled with a thin later of pericardial fluid produced but he serous pericardium. The pericardial fluid helps reduce friction as the heart moves within the pericardium.
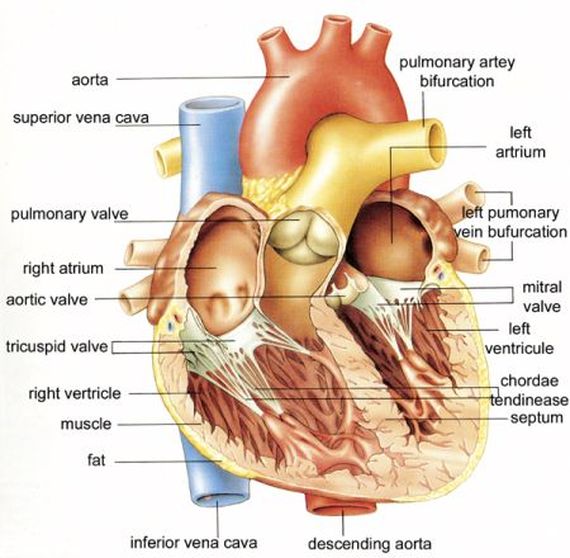
- Six large veins carry blood to the heart. The superior vena cava and inferior vena cava carry blood from the body to the right atrium and four pulmonary veins carry blood from the lungs to the left atrium.
- Two arteries, the pulmonary trunk and the aorta, exit the heart. The pulmonary trunk, arising from the right ventricle, splits into the right and left pulmonary arteries, which carry blood to the lungs. The aorta, arising from the left ventricle, carries blood to the rest of the body.
Heart Valves:
The atrioventricular (AV) valves are located between the right atrium and the right ventricle and between the left atrium and the left ventricle. The AV valve between the right atrium and the right ventricle has three cusps and is called the tricuspid valves. The AV valve between the left atrium and the left ventricle has two cusps and is called the bicuspid valve or mitral valve. These valves allow blood to flow from the atria into the ventricles but prevent it from flowing back into the atria. When the ventricles relax, the higher pressure in the atria forces the AV valves to open and blood flows from the atria into the ventricles. In contrast, when the ventricles contract, blood flows toward the atria and causes the AV valves to close.
Each ventricle contains con-shaped muscular pillars called papillary muscles. These muscles are attached by thin, strong, connective tissue strings called chordae tendineae to the free margins of the cusps of the atrioventricular valves. When the ventricles contract, the papillary muscles contract and prevent the valves from opening into the atria by pulling on the chordae tendineae attached to the valve cusps.
The aorta and pulmonary trunk possess aortic and pulmonary semilunar valves, respectively. Each valve consists of three pocket like semilunar (half-moon-shaped) cusps. When the ventricles contract, the increasing pressure within the ventricles forces the semilunar valves to open. When the ventricles relax, the pressure in the aorta and pulmonary trunk are higher than in the ventricles. Blood flows back from the aorta or pulmonary trunk toward the ventricles and enters the pockets of the cusps, causing them to bulge toward and meet in the center of the aorta or pulmonary trunk, thus closing the vessels and blocking blood flow back into the ventricles.
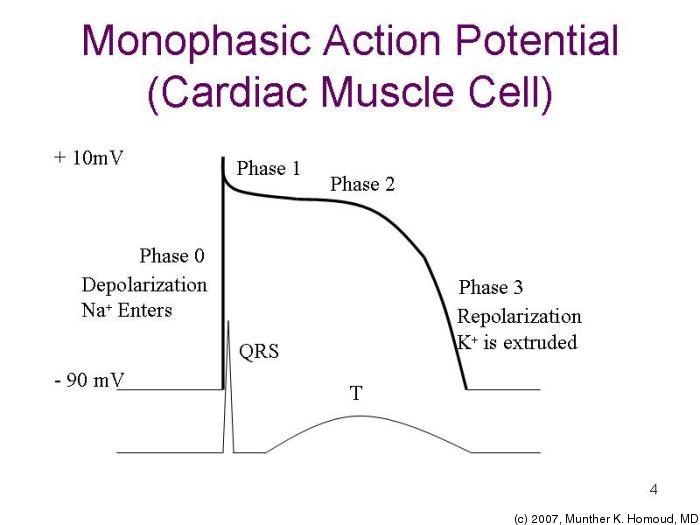
The epicardium, also called the visceral pericardium, is a thin, serious membrane forming the smooth outer surface of the heart. It consists of simple squamous epithelium overlying a layer of loose connective tissue and adipose tissue. The thick, middle layer of the heart, the myocardium, is composed of cardiac muscle cells and is responsible for contraction of the heart chambers. The smooth inner surface of the heart chambers is the endocardium, which consists of simple squamous epithelium over a layer of connective tissue. - Depolarization Phase- Na+ channels open. Ca2+ channels open.
- Plateau Phase- Na+ channels close. Some K+ channels open, causing depolarization. Ca2+ channels are open, producing the plateau by slowing further repolarization.
- Repolarization Phase- Ca2+ channels close. Many K+ channels open.
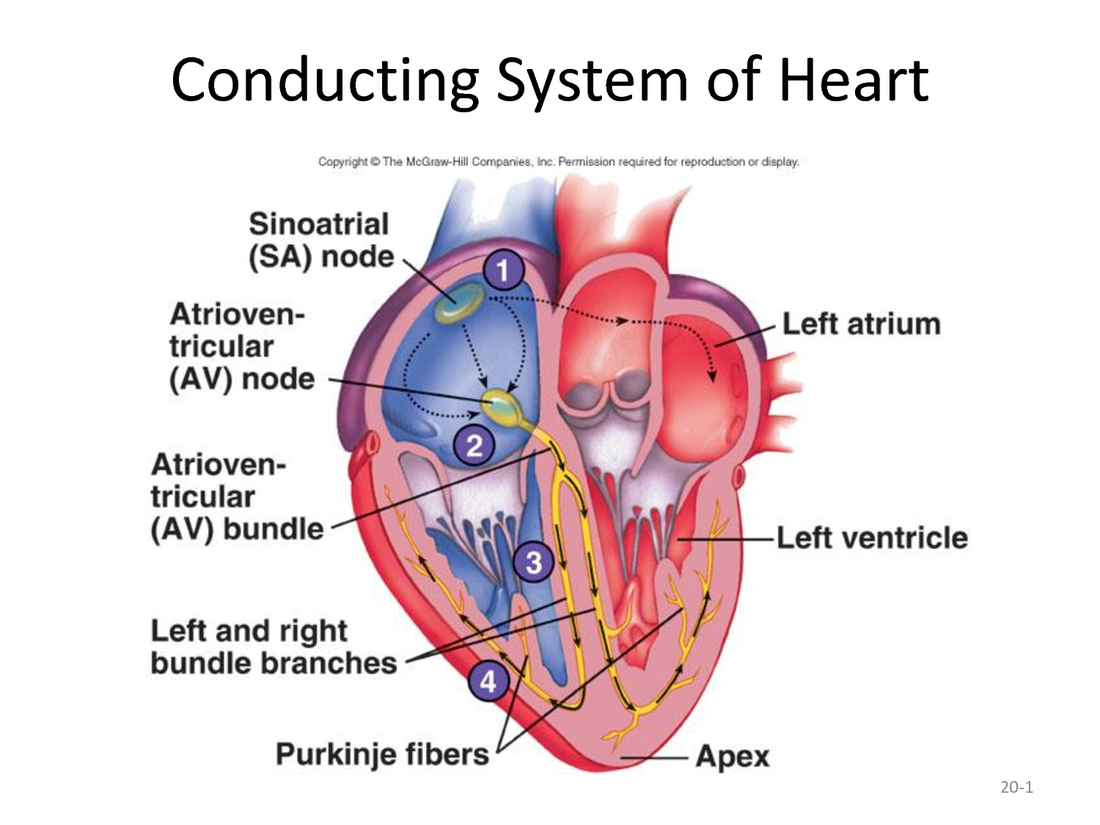
Conduction System of the Heart: - Action potentials originate in the sinoatrial (SA) node and travel across the wall of the atrium (arrows) from the SA doe to the atrioventricular (AV) node.
- Action potentials pass through the AV node and along the atrioventricular (AV) bundle, which extends from the AV node, through the fibrous skeleton, into the inter ventricular septum.
- The AV bundle divides into right and left bundle branches, and action potentials descend to the apex of each ventricle along the bundle branches.
- Action potentials are carried but he Purjinke fibers from the bundle branches to the ventricular walls.
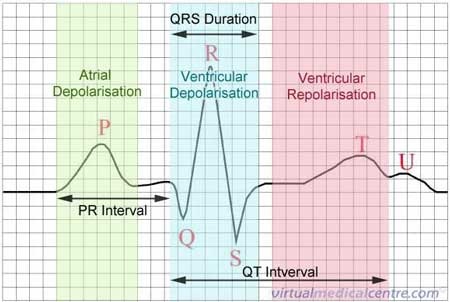
Small electrical changes resulting from action potentials in all of the cardiac muscle cell are recorded by an electrocardiogram (ECG or EKG). The normal ECG consists of a P wave, a QRS complex, and a T wave. the P wave results from depolarization of the atrial myocardium, and the beginning of the P wave precedes the onset of atrial contraction. The QRS complex consists of three individual waves: the Q, R, and S waves. The QRS complex results from depolarization of the ventricles, and the beginning of the QRS complex precedes ventricular contraction. The T wave represents depolarization of the ventricles, and the beginning of the T wave precedes ventricular relaxation. A wave representing depolarization of the atria cannot be seen because it occurs during the QRS complex.
Blood helps maintain homeostasis in several ways: - Transport of gases, nutrients, and waste products.
- Transport of processed molecules.
- Transport of regulatory molecules.
- Regulation of pH and osmosis.
- Maintenance of body temperature.
- Protection against foreign substances.
- Clot formation.
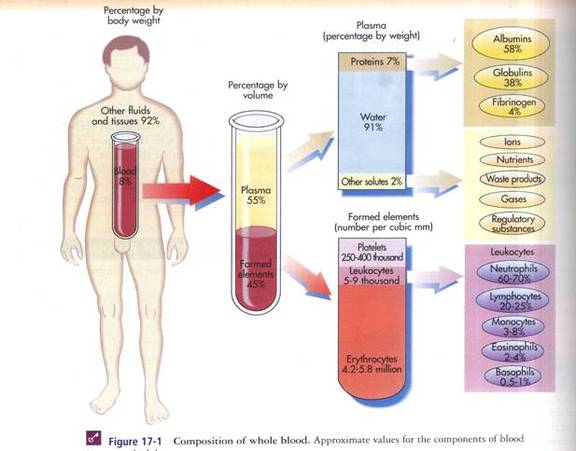
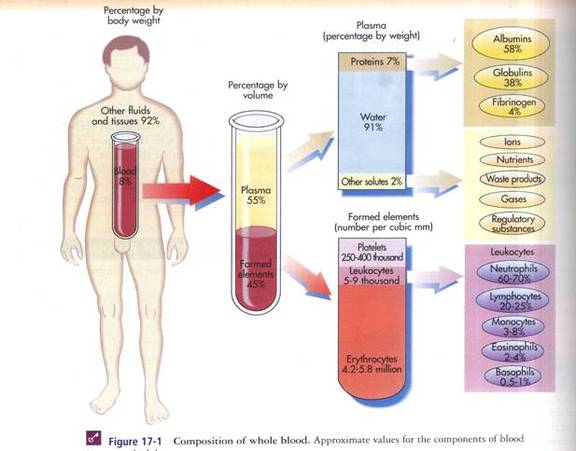
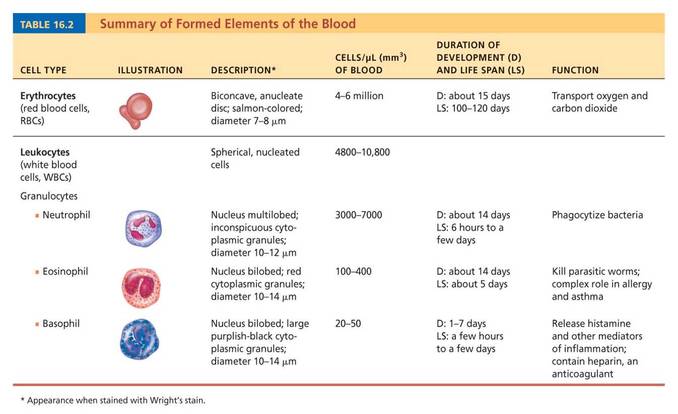
Composition of Blood
Composition of Blood:- Plasma- The liquid matrix
- Formed Elements- cells and cell fragments
- Plasma contains dissolved proteins. Plasma proteins include albumin, globulins, and fibrinogen.
- Albumin- makes up 58% of the plasma proteins.
- Globulin- accounts for 38% of the plasma proteins. Some globulins such as antibodies and complement, are part of the immune system. Other globulins and albumin function as transport molecules because they bind to molecules such as hormones and carry them in the blood throughout the body.
- Fibrinogen- is a clotting factor that constitutes 4% of plasma proteins. Activation of clotting factor that constitutes 4% of plasma proteins. Activation of clotting factors results in the conversion of fibrinogen to fibrin, a threadlike protein that forms blood clots.
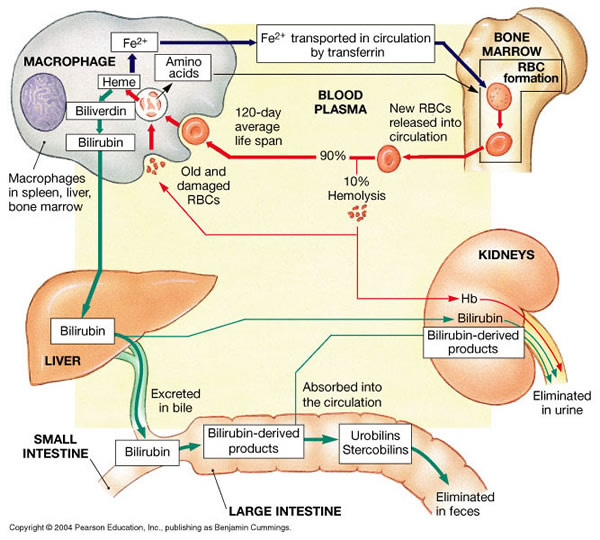
Hemoglobin Breakdown:- In macrophages, the glob in part of hemoglobin is broken down to individual amino acids and metabolized or used to build new proteins.
- The heme of hemoglobin releases iron. The heme is converted into bilirubin.
- Blood transports iron to the red bone marrow, where it is used to produce new hemoglobin.
- blood transports bilirubin to the liver.
- Bilirubin is excreted as part of the bile into the small intestine. Some bilirubin derivatives contribute to the color of feces.
- Other bilirubin derivatives are reabsorbed from the intestine into the blood and excreted from the kidneys in the urine.
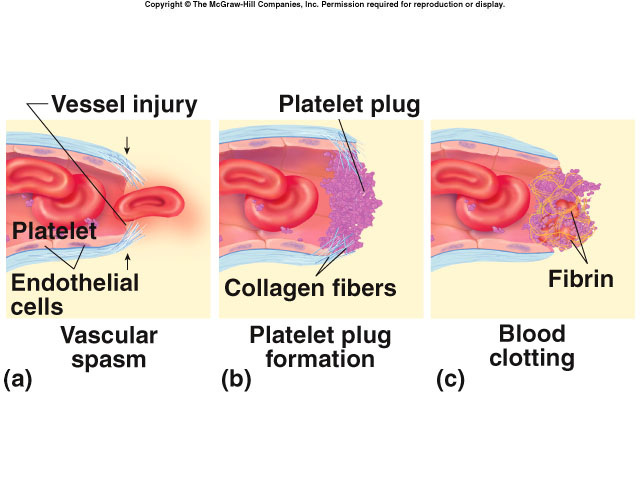
Blood loss is minimized in three ways:- Vascular Spasm- Is an immediate but temporary constriction of a blood vessel that results when smooth muscle within the wall of the vessel contracts.
- Platelet Plug- Is an accumulation of platelets that can seal up a small break in a blood vessel. Platelet plug formation is described in a series of steps: First, platelets stick to the collaged exposed by blood vessel damage; this phenomenon is called platelet adhesion. Most platelet adhesion is mediated through von Willebrand factor, a protein produced and secreted by blood vessel endothelial cells. Von Willebrand factor forms a bridge between collagen and platelets by binding to platelet surface receptors and collagen. After platelets adhere to collagen, they become activated, change shape, and release chemicals.
- Blood Clotting: Results in the formation of a clot. A clot is a network of threadlike protein fibers, called fibrin, that traps blood cells, platelets, and fluid.
- Clot formation is a complex process involving many chemical reactions, but it can be summarized in three stages:
- The chemical reactions can be started in two ways: a.) inactive clotting factors come in contact with exposed connective tissue, resulting in their activation, or b.) chemicals, such as thromboplastin, are released from injured tissues, causing activation of clotting factors. After the initial clotting factors are activated, they in turn activate other clotting factors. A series of reactions results in which each clotting factor activates the next until the clotting factor prothrombinase, or prothrombin activator is formed.
- Prothrombinase converts an inactive clotting factor called prothrombin to its active form, thrombin.
- Thrombin converts the inactive clotting factor fibrinogen to its active form fibrin.
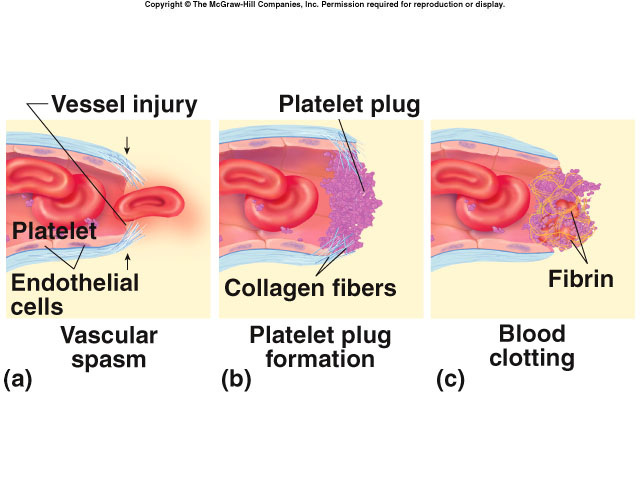
Three preventions of blood loss
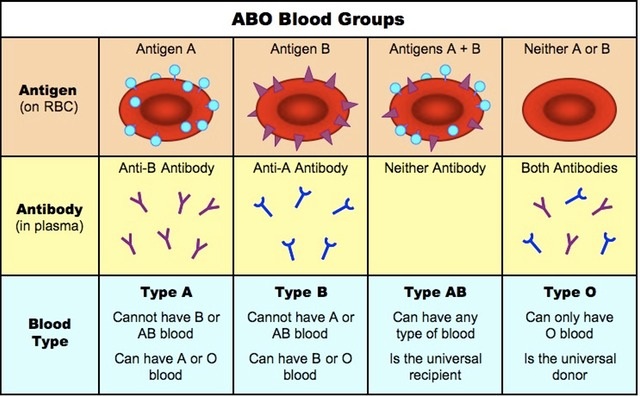
The ABO blood group system is used to categorize human blood. ABO antigens appear on the surface of red blood cells. Type A blood has type A antigens, type B blood has type B antigens, type AB blood has both types of antigens, and type O blood has neither A nor B antigens. In addition, plasma from type A blood contains anti-B antibodies, which act against type B antigens; plasma from type B blood contains anti-A antibodies, which act against type A antigens. Type AB blood plasma has neither type of antibody, and type O blood plasma has both anti-A and anti-B antibodies.
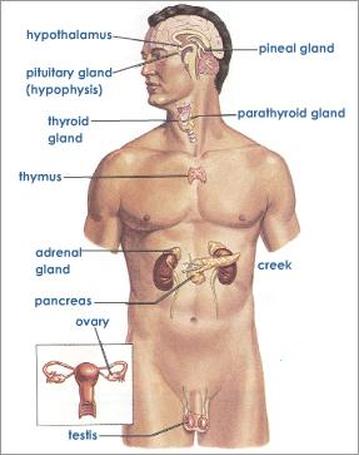
Classes of Chemical Messengers: - Autocrine chemical messengers- An autocrine chemical messenger stimulates the cell that originally secreted it.
- Paracrine chemical messengers- Paracrine chemical messengers act locally on nearby cells. These chemical messengers are secreted by one cell type into the extracellular fluid and affect surrounding cells.
- Neurotransmitters- Neurotransmitters are chemical messengers secreted by neurons that activate an adjacent cell, whether it is another neuron, a muscle cell, or a glandular cell.
- Endocrine chemical messengers- Endocrine chemical messengers are secreted into the bloodstream by certain glands and cells, which together constitute the endocrine distant from their source.
Functions of the Endocrine System: - Metabolism.
- Control of food intake and digestion.
- Tissue development.
- Ion regulation.
- Water regulation.
- heart rate an blood pressure regulation.
- Control of blood glucose and other nutrients.
- Control of reproductive functions.
- Uterine contractions and milk release.
- Immune system regulation.
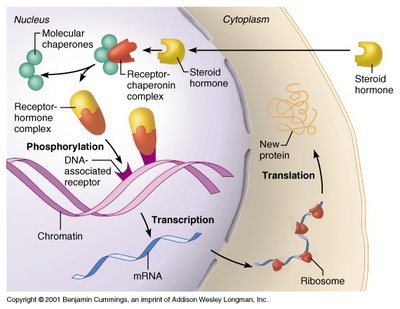
Lipid-Soluble Hormones
Lipid- soluble hormones are non polar, and include steroid hormones, thyroid hormones, and fatty acid derivative hormones, such as certain eicosanoids.
Transport of Lipid-Soluble Hormones
Because of their small size and low solubility in aqueous fluids, lipid-soluble hormones travel in the bloodstream attached to binding proteins, proteins that transport the hormones.
Water-Soluble Hormones
Water-soluble hormones are polar molecules; they include protein hormones, peptide hormones, and most amino acid derivative hormones.
Transport of Water-Soluble Hormones
Because water-soluble hormones can dissolve in blood, many circulate as free hormones, meaning that most of them dissolve directly into the blood and are delivered to their target tissue without attaching to a binding protein.
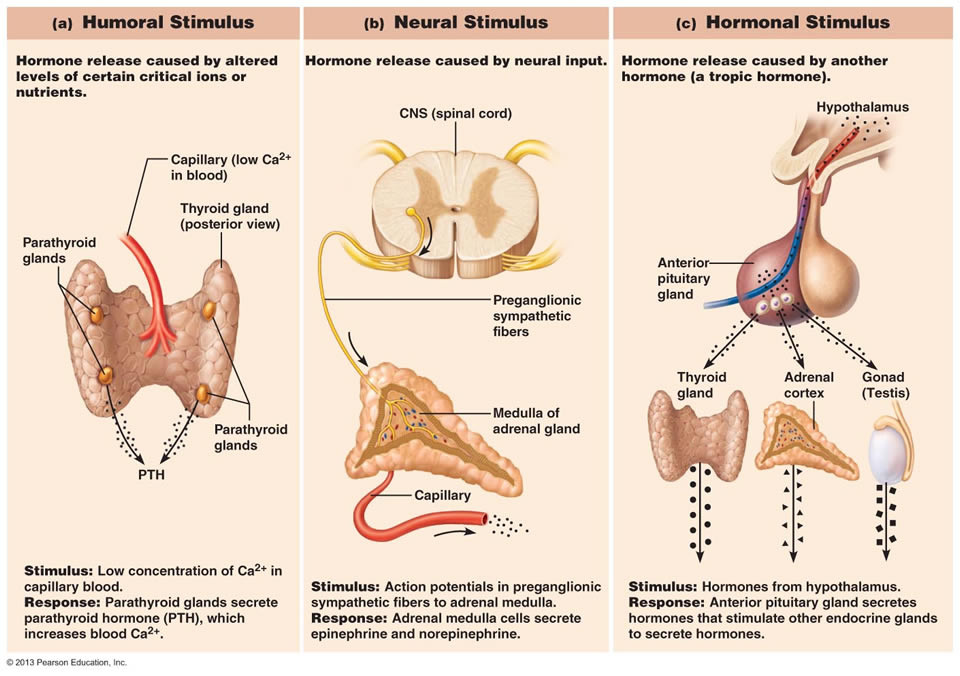
Stimulation of Hormone Release by Humoral Stimuli:
Blood-borne molecules can directly stimulate the release of some hormones. These molecules are referred to as humoral stimuli because they circulate in the blood. These hormones are sensitive to the the blood levels of a particular substance such as glucose, calcium, sodium.
Stimulation of Hormone Release by Neural Stimuli:
Following action potentials, neurons release a neurotransmitter into the synapse with the cells that produce the hormone.
Stimulation of Hormone Release by Hormonal Stimuli:
It occurs when a hormone is secreted that, in turn, stimulates the secretion of other hormones. The most common examples are hormones from the anterior pituitary gland, called tropic hormones. Negative Feedback by Hormones:- The anterior pituitary gland secretes a tropic hormone, which travels in the blood to the target endocrine cell.
- The hormone from the target endocrine cell travels to its target.
- The hormone from the target endocrine cell also has a negative-feedback effect on the anterior pituitary and hypothalamus and decreases secretion of the tropic hormone.
Positive Feedback by Hormones:- The anterior pituitary gland secretes a tropic hormone, which travels in the blood to the target endocrine cell.
- The hormone from the target endocrine cell travels to its target.
- The hormone from the target endocrine cell also has a positive-feedback effect on the anterior pituitary and increases secretion of the tropic hormone.
Positive and Negative Feedback by Hormones
Nuclear Receptor Model: - Lipid-soluble hormones diffuse through the plasma membrane.
- Lipid-soluble hormones bind to cytoplasmic receptors and travel to the nucleus or bind to nuclear receptors. Some lipid-soluble hormones bind receptors in the cytoplasm and then move into the nucleus.
- The hormone-receptor complex binds to a hormone response element on the DNA, acting as a transcription factor.
- The biding of the hormone-receptor complex to DNA stimulates the synthesis of messenger RNA (mRNA), which codes for specific proteins.
- The mRNA leaves the nucleus, passes into the cytoplasm of the cell, and binds to ribosomes, where it directs the synthesis of specific proteins.
- The newly synthesized proteins produce the cell's response to the lipid-soluble hormones- for example, the secretion of a new protein.
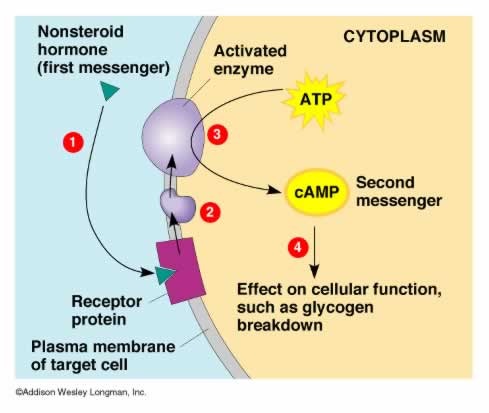
Membrane-Bound Receptors Activate G Proteins- After a water-soluble hormone binds to its receptor, the G protein is activated.
- The activated alpha subunit, with GTP bound to it, binds to and activates an adenylate cyclase enzyme so that it converts ATP to cAMP.
- The cAMP can activate protein kinase enzymes, which phosphorylate specific enzymes activating them. The chemical reactions catalyzed by the activated enzymes produce the cell's response.
- Phosphodiesterase enzymes inactivate cAMP by converting cAMP to AMP.
|





 RSS Feed
RSS Feed