Functions of the Heart:
- Generating blood pressure.
- Routing blood.
- Ensuring one-way blood flow.
- Regulating blood supply.
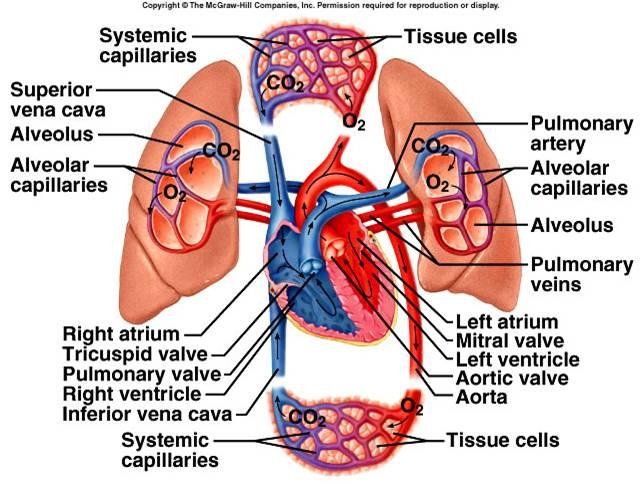
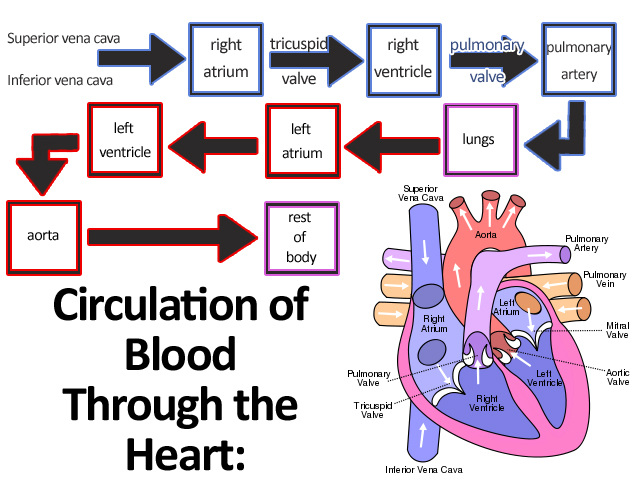
The right side of the heart pumps blood to the lungs and back tot he left side of the heart through vessels of the pulmonary circulation. The left side of the heart pumps blood to all other tissues of the body and back to the right side of the heart through vessels of the systemic circulation.
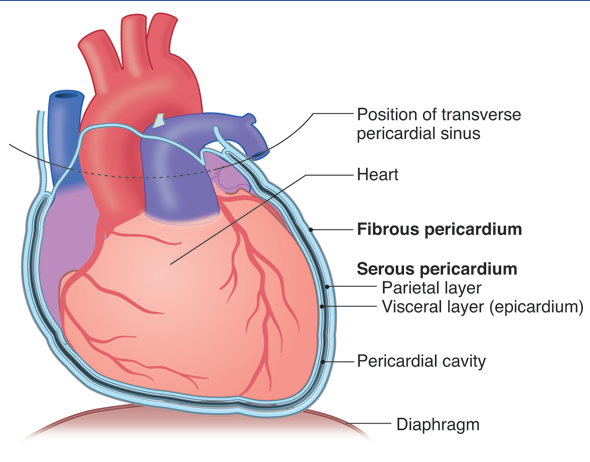
Pericardium:
The heart lies in the pericardial cavity. The pericardial cavity is formed by the pericardium, or pericardial sac, tissues that surround the heart and anchor it within the mediastinum. The pericardium consists of two laters: the fibrous pericardium and the serous pericardium. The portion of the serious pericardium lining the fibrous pericardium is the parietal pericardium, whereas the portion covering the heart surface is the visceral pericardium, or epicardium. The parietal and visceral pericardia are continuous with each other where the great vessels enter or leave the heart. The pericardial cavity, located between the visceral and parietal pericardia, is filled with a thin later of pericardial fluid produced but he serous pericardium. The pericardial fluid helps reduce friction as the heart moves within the pericardium.
The heart lies in the pericardial cavity. The pericardial cavity is formed by the pericardium, or pericardial sac, tissues that surround the heart and anchor it within the mediastinum. The pericardium consists of two laters: the fibrous pericardium and the serous pericardium. The portion of the serious pericardium lining the fibrous pericardium is the parietal pericardium, whereas the portion covering the heart surface is the visceral pericardium, or epicardium. The parietal and visceral pericardia are continuous with each other where the great vessels enter or leave the heart. The pericardial cavity, located between the visceral and parietal pericardia, is filled with a thin later of pericardial fluid produced but he serous pericardium. The pericardial fluid helps reduce friction as the heart moves within the pericardium.
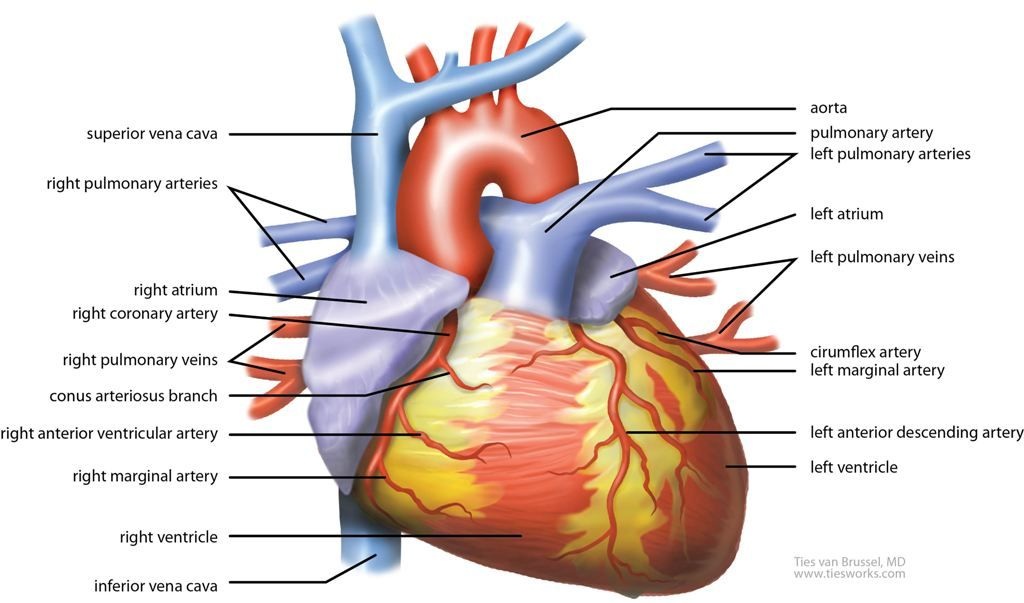
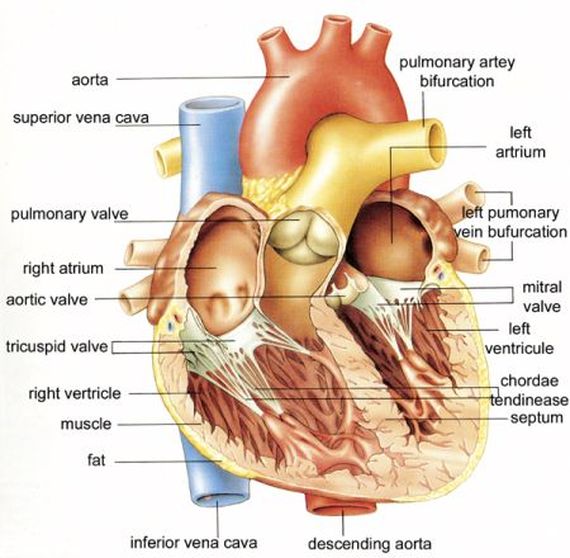
- Six large veins carry blood to the heart. The superior vena cava and inferior vena cava carry blood from the body to the right atrium and four pulmonary veins carry blood from the lungs to the left atrium.
- Two arteries, the pulmonary trunk and the aorta, exit the heart. The pulmonary trunk, arising from the right ventricle, splits into the right and left pulmonary arteries, which carry blood to the lungs. The aorta, arising from the left ventricle, carries blood to the rest of the body.
Heart Valves:
The atrioventricular (AV) valves are located between the right atrium and the right ventricle and between the left atrium and the left ventricle. The AV valve between the right atrium and the right ventricle has three cusps and is called the tricuspid valves. The AV valve between the left atrium and the left ventricle has two cusps and is called the bicuspid valve or mitral valve. These valves allow blood to flow from the atria into the ventricles but prevent it from flowing back into the atria. When the ventricles relax, the higher pressure in the atria forces the AV valves to open and blood flows from the atria into the ventricles. In contrast, when the ventricles contract, blood flows toward the atria and causes the AV valves to close.
Each ventricle contains con-shaped muscular pillars called papillary muscles. These muscles are attached by thin, strong, connective tissue strings called chordae tendineae to the free margins of the cusps of the atrioventricular valves. When the ventricles contract, the papillary muscles contract and prevent the valves from opening into the atria by pulling on the chordae tendineae attached to the valve cusps.
The aorta and pulmonary trunk possess aortic and pulmonary semilunar valves, respectively. Each valve consists of three pocket like semilunar (half-moon-shaped) cusps. When the ventricles contract, the increasing pressure within the ventricles forces the semilunar valves to open. When the ventricles relax, the pressure in the aorta and pulmonary trunk are higher than in the ventricles. Blood flows back from the aorta or pulmonary trunk toward the ventricles and enters the pockets of the cusps, causing them to bulge toward and meet in the center of the aorta or pulmonary trunk, thus closing the vessels and blocking blood flow back into the ventricles.
The atrioventricular (AV) valves are located between the right atrium and the right ventricle and between the left atrium and the left ventricle. The AV valve between the right atrium and the right ventricle has three cusps and is called the tricuspid valves. The AV valve between the left atrium and the left ventricle has two cusps and is called the bicuspid valve or mitral valve. These valves allow blood to flow from the atria into the ventricles but prevent it from flowing back into the atria. When the ventricles relax, the higher pressure in the atria forces the AV valves to open and blood flows from the atria into the ventricles. In contrast, when the ventricles contract, blood flows toward the atria and causes the AV valves to close.
Each ventricle contains con-shaped muscular pillars called papillary muscles. These muscles are attached by thin, strong, connective tissue strings called chordae tendineae to the free margins of the cusps of the atrioventricular valves. When the ventricles contract, the papillary muscles contract and prevent the valves from opening into the atria by pulling on the chordae tendineae attached to the valve cusps.
The aorta and pulmonary trunk possess aortic and pulmonary semilunar valves, respectively. Each valve consists of three pocket like semilunar (half-moon-shaped) cusps. When the ventricles contract, the increasing pressure within the ventricles forces the semilunar valves to open. When the ventricles relax, the pressure in the aorta and pulmonary trunk are higher than in the ventricles. Blood flows back from the aorta or pulmonary trunk toward the ventricles and enters the pockets of the cusps, causing them to bulge toward and meet in the center of the aorta or pulmonary trunk, thus closing the vessels and blocking blood flow back into the ventricles.
The epicardium, also called the visceral pericardium, is a thin, serious membrane forming the smooth outer surface of the heart. It consists of simple squamous epithelium overlying a layer of loose connective tissue and adipose tissue. The thick, middle layer of the heart, the myocardium, is composed of cardiac muscle cells and is responsible for contraction of the heart chambers. The smooth inner surface of the heart chambers is the endocardium, which consists of simple squamous epithelium over a layer of connective tissue.
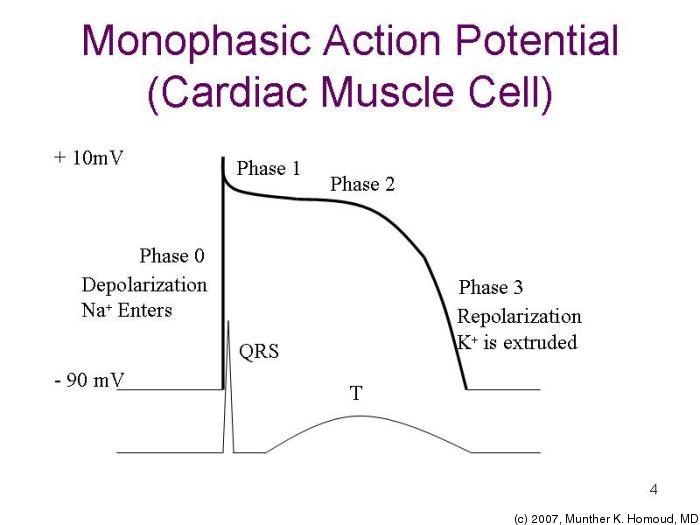
- Depolarization Phase- Na+ channels open. Ca2+ channels open.
- Plateau Phase- Na+ channels close. Some K+ channels open, causing depolarization. Ca2+ channels are open, producing the plateau by slowing further repolarization.
- Repolarization Phase- Ca2+ channels close. Many K+ channels open.
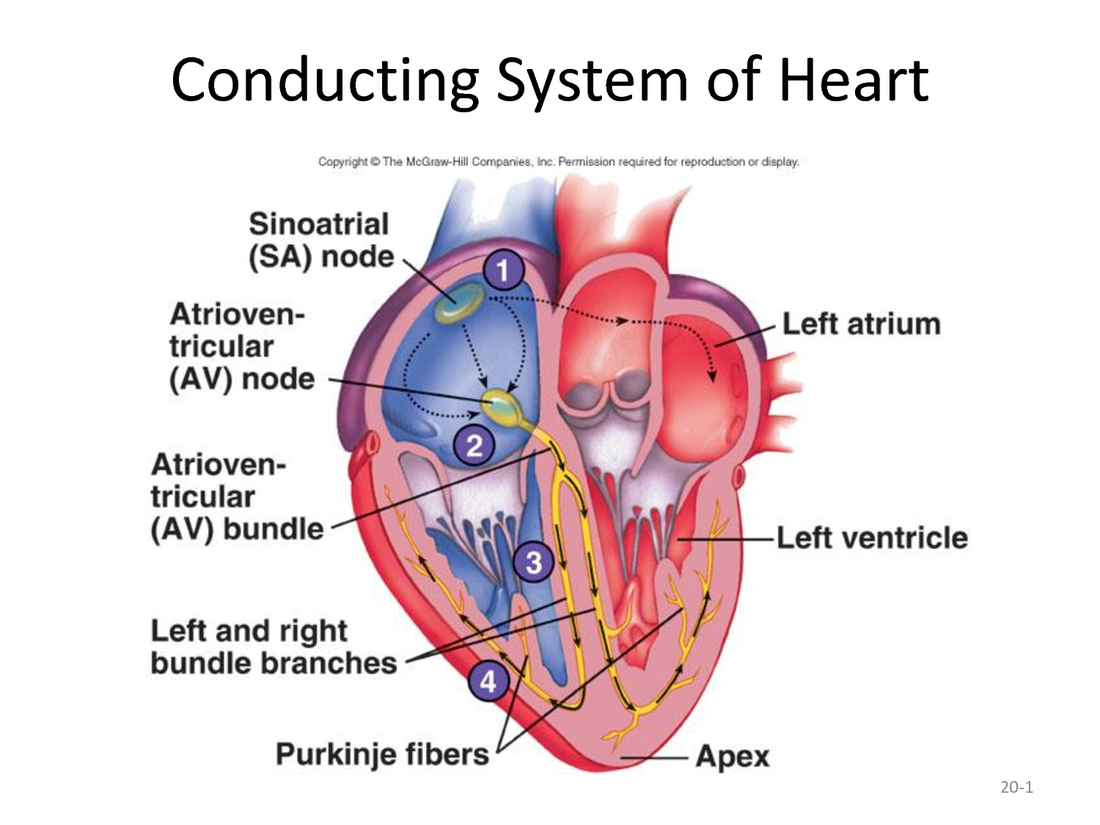
Conduction System of the Heart:
- Action potentials originate in the sinoatrial (SA) node and travel across the wall of the atrium (arrows) from the SA doe to the atrioventricular (AV) node.
- Action potentials pass through the AV node and along the atrioventricular (AV) bundle, which extends from the AV node, through the fibrous skeleton, into the inter ventricular septum.
- The AV bundle divides into right and left bundle branches, and action potentials descend to the apex of each ventricle along the bundle branches.
- Action potentials are carried but he Purjinke fibers from the bundle branches to the ventricular walls.
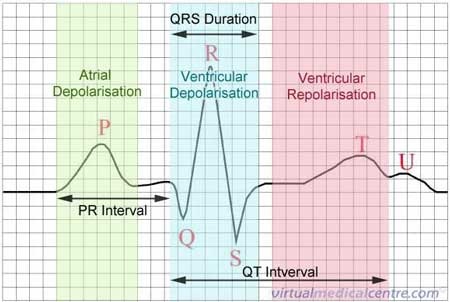
Small electrical changes resulting from action potentials in all of the cardiac muscle cell are recorded by an electrocardiogram (ECG or EKG). The normal ECG consists of a P wave, a QRS complex, and a T wave. the P wave results from depolarization of the atrial myocardium, and the beginning of the P wave precedes the onset of atrial contraction. The QRS complex consists of three individual waves: the Q, R, and S waves. The QRS complex results from depolarization of the ventricles, and the beginning of the QRS complex precedes ventricular contraction. The T wave represents depolarization of the ventricles, and the beginning of the T wave precedes ventricular relaxation. A wave representing depolarization of the atria cannot be seen because it occurs during the QRS complex.
 RSS Feed
RSS Feed